Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de la Facultad de Medicina Humana
Print version ISSN 1814-5469On-line version ISSN 2308-0531
Rev. Fac. Med. Hum. vol.21 no.1 Lima Jan-Mar 2021
http://dx.doi.org/10.25176/rfmh.v21i1.3607
Clinical case
Clinical spectrum of systemic lupus erythematosus in children. Case report.
1Hospital Nacional Edgardo Rebagliati Martins - EsSalud, Lima - Peru.
Systemic lupus erythematosus is an autoimmune disease with multisystem involvement, an alternating clinical course, and which constitutes a diagnostic challenge, with a greater disease activity in the pediatric age group, which also darkens its prognosis. In this article, we report the case of a ten year old female patient who debuted with systemic lupus erythematosus with gastrointestinal, renal and hematological involvement; the chronic course coupled with the varied clinical spectrum suggested the diagnostic possibility.
Key words: lupus erythematosus; Children; Enteritis; Nephritis; Anemia (source: MeSH NLM).
INTRODUCTION
ESystemic lupus erythematosus (SLE) is an autoimmune disease with multisystemic involvement and recurrent chronic course, which is associated with a considerable morbidity and mortality1.
Pediatric SLE (cSLE) is a rare disease with a median age of presence between 11 and 12 years; being quite uncommon in children under five years, it has a majority prevalence in the female sex2. The etiology is unknown. It is characterized by inflammatory lesions localized in many organs, especially in skin, joints, kidneys and serous membranes3. The varied clinical spectrum of presence, together with the fact that it shares characteristics of other diseases, often makes early diagnosis4difficult. Likewise, cSLE follows a more serious clinical course compared to its presence in adults, with greater disease activity and a faster accumulation of multi-organ damage5.
The objective of this report is to present the heterogeneous clinical spectrum of SLE in a pediatric patient reviewing relevant aspects for her diagnosis.
CASE REPORT
Ten-year-old female patient with a family history of SLE, diagnosed with hypothyroidism in February 2020 and treated with levothyroxine. Eight months prior to this diagnosis, the patient presented dermal lesions in the armpits. Two weeks later, hematuria and edema were added in the lower limbs and arthralgia. At the fourth week of illness, she had an intermittent fever. She was evaluated and treated by a private doctor with antibiotics for probable urinary tract infection, without clinical improvement. Weeks later, the symptoms persisted. The arthralgia intensified and hindered the mobilization. She was taken to the former hospital where she was admitted through emergency, being hospitalized for study. Patient undergoes creatinine elevation, proteinuria, severe hemolytic anemia with positive direct Coombs test and coagulopathy, which requires transfusion support and coagulopathy correction. Due to the high suspicion of diagnosis of SLE, ANA is requested which results positive and treatment with prednisone and hydroxychloroquine is initiated. The patient is discharged with treatment and indication of outpatient care.
The patient enters again through emergency as she presented a decompensation by an underlying condition, with signs of shock, uncontrolled vomiting and anasarca. The analysis shows severe anemia with positive direct Coombs, hypokalemia, prolongation of coagulation times, proteinuria in nephrotic range, hematuria and consumption of c3 and C4. The specific detection of various autoantibodies is detailed inTable 1.
Ultrasound shows hepatosplenomegaly and abundant free fluid in the abdomen associated with distension of intestinal loops. Thoracoabdominal tomography reveals the presence of intestinal subocclusion signs, dilatation of jejunal loops, mild pleural effusion and mild pericardial effusion.
Therefore, the patient is treated with multisystemic involvement of lupus (hematological, renal and gastrointestinal). Hemodynamic stabilization and initiation of intravenous methylprednisolone pulses are carried out.
Renal biopsy studies were supplemented with a diagnosis of lupus nephritis class IV. The patient receives induction treatment with cyclophosphamide. With persistent vomiting, resulting in normal intestinal transit, duodenal biopsy is reported with a highly suggestive diagnosis of autoimmune enteropathy.
Progressive disease control is achieved with prednisone and hydroxychloroquine. Patient is discharged after 5 months.
| Antibodies | Reference value | Result |
|---|---|---|
| Antinuclear antibody (ANA) | Positive Title: 1/1280 | |
| Anti-Smith antibody (Sm). (U/ml) | <12 | 16.1 |
| Anti Ro | Negative | |
| Anti La | Negative | |
| Anti RNP | Negative | |
| Anti Jo-1 | Negative | |
| Anti Scl-70 | Negative | |
| Anticardiolipin IgM antibodies (MPL/ml) | <15 | 22,9 |
| Anticardiolipin IgG antibodies (MPL/ml) | <17 | 11,5 |
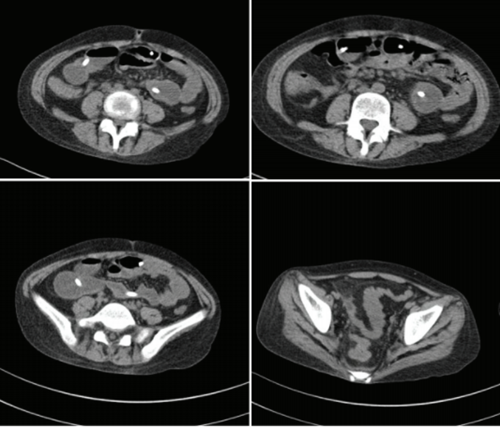
Figure 1. Intestinal loops dilated and with liquid contents, of apparently preserved wall to the part of ileal intestine. Ascending colon part of transverse sigmoid descending colon and rectal blister of apparently collapsed appearance with thickening of the wall without evidence of haustration to rule out a inflammatory process.
DISCUSSION
In relation to the clinical phenotype, most studies have reported substantial differences between cSLE and the adult onset disease, showing a higher frequency of renal, hematological and neuropsychiatric involvement in pediatric patients3.
It is recognized that the juvenile onset SLE has a more active course of the disease compared to the onset disease in adulthood, as occurred in this case. Patients have a worse long-term survival6.
Lupus enteritis can be expressed as the first gastrointestinal manifestation. It is rare, the prevalence reaches 0.2-2% in the total of patients with SLE, and it requires a high index of suspicion that includes abdominal pain (97%), vomiting (42%), and diarrhea (32%). The aforementioned is complemented with images, such as the abdominal tomography which describes the thickening diffuse from the bowel wall, dilatation of bowel loops, thickening, splanchnic hypervascularization and increased attenuation of mesenteric and ascites fat.8,9,10In this case report, the patient presents a clinical picture, complementary imaging examinations and duodenal biopsy with a highly suggestive diagnosis of autoimmune enteropathy.
Likewise, anemia is the most common hematological manifestation of SLE in children and adolescents. Usually, this is a microcytic anemia of chronic disease7. Although rare in SLE, Coombs positive hemolytic anemia occurs most commonly in the infantile form of the disease. If it is the first manifestation, it may appear several years before the diagnosis of SLE1,10,11.
CONCLUSION
This case report shows the varied clinical manifestations of SLE in a pediatric patient that constitutes a diagnostic challenge due to its heterogeneous and alternating clinical spectrum. However, the chronic and multisystemic course suggested the diagnostic alert and establishment of the treatment which allowed the progressive control of the disease.
REFERENCIAS BIBLIOGRÁFICAS
1. Harry O, Yasin S, Brunner H. Childhood-Onset Systemic Lupus Erythematosus: A Review and Update. J Pediatr. 2018; 196: 22-30. e2. doi: 10.1016/j.jpeds.2018.01.045 [ Links ]
2. Levy DM, Kamphuis S. Systemic lupus erythematosus in children and adolescents. Pediatr Clin North Am. 2012 Apr;59(2):345-64. doi: 10.1016/j.pcl.2012.03.007. [ Links ]
3. Casado Arroyo R., Lado Lado F. L., Rodríquez Constenla I., Rodríguez López I. Anemia hemolítica autoimmune como forma de presentación de lupus eritematoso sistémico. An. Med. Interna (Madrid) (Internet). 2003 Sep (citado 2020 Oct 18); 20(9 ): 61-61. [ Links ]
4. Costagliola G, Mosca M, Migniorini P, CONSOLINI R (2018) Pediatric systemic lupus erythematosus: learning from longer follow up to adulthood. Front Pediatr 6:144. [ Links ]
5. Kamphuis, S., Silverman, E. Prevalence and burden of pediatric-onset systemic lupus erythematosus. Nat Rev Rheumatol 6, 538-546 (2010). https://doi.org/10.1038/nrrheum.2010.121. [ Links ]
6. Oni, L., Wright, R.D., Marks, S. et al. Kidney outcomes for children with lupus nephritis. Pediatr Nephrol (2020). https://doi.org/10.1007/s00467-020-04686-1 [ Links ]
7. Levy DM. Childhood-onset systemic lupus erythematosus (SLE): clinical manifestations and diagnosis. Available at https://www.uptodate.com/contents/ systemic-lupus-erythematosus-sle-inchildren-clinical-manifestations-anddiagnosis. [ Links ]
8. Barrera O. Manuel, Barrera M. Rodrigo, de la Rivera V. Matías, Vela U. Javier, Mönckeberg F. Gustavo. Enteritis lúpica como manifestación inicial de lupus eritematoso sistémico. Caso clínico. Rev. méd. Chile. 2017 oct; 145(10): 1349-1352. [ Links ]
9. Adalberto Gonzalez, Vaibhav Wadhwa, Fayssa Salomon, Jeevna Kaur, Fernando J Castro. (2019) Lupus enteritis as the only active manifestation of systemic lupus erythematosus: A case report. World Journal of Clinical Cases 7:11, pages 1315-1322. [ Links ]
10. Sonmez HE, Karhan AN, Batu ED, et al.Gastrointestinal system manifestations in juvenile systemic lupus erythematosus. Clin Rheumatol. 2017;36:1521-1526. [ Links ]
11. Velo-García A Guerreiro S Isenberg D. The diagnosis and management of the haematological manifestations of lupus. J Autoimm. 2016;139-160. [ Links ]
Received: January 02, 2021; Accepted: January 10, 2021











 text in
text in 


