Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.21 no.3 Lima jul./set. 2021
http://dx.doi.org/10.25176/rfmh.v21i1.3408
Original article
Family cohesion and time of hospitalization in patients with mental disorders in a hospital in Lambayeque, Peru
1Escuela de Medicina, Universidad Católica Santo Toribio de Mogrovejo. Chiclayo, Perú
2Hospital Regional Lambayeque. Lambayeque, Perú
3Centro especializado de salud mental comunitario. Chiclayo, Perú
Mental disorders represent about 22% of the total burden of disease, and family support plays an important role in the length of hospitalization time in these patients. We described the family cohesion and the time of hospitalization in patients of the psychiatric service of the Hospital Nacional Almanzor Aguinaga Asenjo (H.N.A.A.A) during 2019. This is a cross-sectional descriptive census-type study, in which a questionnaire of 11 questions on family cohesion was applied. Sociodemographic and clinical data were collected through a data collection form. 60 patients were surveyed, the median age was 50 years, the most frequent diagnosis was schizophrenia; most are female, not working and are single. The median length of hospitalization was 12.5 days. Those who respond positively to questions tend to stay longer.
Keywords: support systems; hospitalization; mental disorders. (Source: MESH - NLM)
INTRODUCTION
Family is the main source of support1in whom we rely on in moments of crisis and facing a mental disorder affects the family unit, meaning, what happens to one member resonates in all the other family members.2 Several diverse studies exist that show that family cohesion plays an important role as co-adjuvant in the recovery process of patients with mental disorders3, this favors less relapses, lower drug doses, lower symptom severity3and a better quality of life4. Likewise, the burden and stress, of the family member or caretaker3, in this group of psychiatric patients, is reflected in their abandonment in public hospitals particularly in countries with high poverty rates2. Family cohesion influences the time of hospital stay, since patients with socio-familiar support are hospitalized for shorter duration5and have less hospital admissions in comparison with low family cohesion6. Psychiatry is one of the areas that family and social factors have more influence, becoming a protective factor for shorter duration and lower complication of hospital stay1, therefore, an important relationship exists between family cohesion and hospitalization1-5. However, in our reality there exist few studies on mental health related to these variables, therefore, we propose describing family cohesion and time of hospitalization in patients with mental disorders in the psychiatry service of Hospital Almanzor Aguinaga Asenjo, Chiclayo, Peru. Moreover, describe the psychiatric disorders of patients admitted in the psychiatry service in the year 2019, describe family cohesion that exists in hospitalized patients in the psychiatric service, define the average time of hospitalization in the psychiatric service and, lastly, identify the sociodemographic aspects (sex, age, origin, educational level, diagnosis, occupation and marital status) of the patients hospitalized in the psychiatric service.
THE STUDY
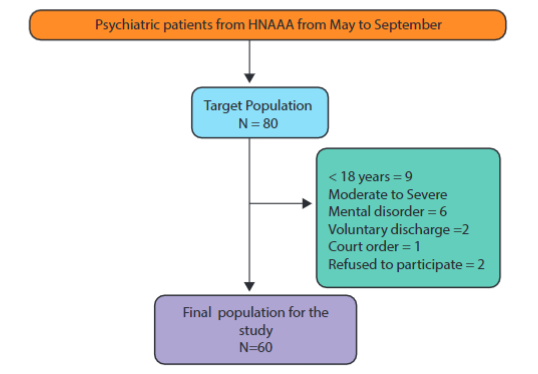
We performed a descriptive, cross-sectional study with a census sampling. The target population were 80 patients of which 60 met the inclusion criteria and 20 were excluded, 9 of which were under 18 years of age, 6 with moderate-severe mental disorder, 4 with voluntary discharge, 1 with admission per court order, and 2 refused to participate (Figure 1). They were treated between the months of May to September of 2019 in the hospitalization area of the Psychiatric Service of the H.N.A.A.A. Patients that were clinically stable were excluded, meaning fit and stable according to the evaluation performed by the medical specialist and that were under medical discharge. We did not consider patients with neurocognitive decline, those abandoned by their family, with admission per court order, under 18 years of age, with voluntary discharge and those who refused to participate in the study.
A questionnaire was used and it was made up of 11 questions, related to family cohesion, drawn from the manual belonging to the Epidemiological Study of Mental Health in Metropolitan Lima and Callao - 2012 edition, which was adapted and validated for the population in Lima by the Instituto Nacional de Salud Mental Honorio Delgado - Hideyo Noguchi.6,7The 11 questions were validated qualitatively by three expert psychiatrists from the city of Chiclayo, who evaluated the clarity , relevance and pertinence of each item. We had access to clinical histories in order to obtain the duration of hospitalization, sociodemographic data, which is information that was transcribed to the data collection sheet. Family cohesion data was obtained from the patient interview. All the information mentioned was stored in a data base using the Microsoft Excel 2013 version 15,0 program spreadsheet. The numeric variables were described using the median and interquartile range through the SPSS version 25 program and the categorical variables were described as absolute and relative rates. Tables were used for the sociodemographic and clinical variables. We obtained the approval of the Ethics Committee of the Universidad de Santo Toribio de Mogrovejo and of the H.N.A.A.A. The information regarding the study was offered to the patients and their family members in case they were present. The patients that accepted to participate in the study signed the informed consent. The study posed minimal risks given that the psychiatric patients were a vulnerable population.
FINDINGS
60 people were surveyed, in which the family cohesion rate was searched from the psychiatric patient perspective and the hospitalization time in the psychiatric service of the H.N.A.A.A. We found that in psychiatric patients the median age was 50 years (RI: 32-58 years), the majority were of the feminine sex, almost all originating from Lambayeque, the predominant education level was complete high school and higher education. Furthermore, we found that the majority of the patients were not employed (46/60), were single (38/60), and presented schizophrenia as the most frequent diagnosis (seeTable 1).
Table 1. Sociodemographic and clinical variables of the psychiatric patients from H.A.A.A.
| Sociodemographic and clinical variables | n | % | |
|---|---|---|---|
| Sex | |||
| Feminine | 32 | 53,3% | |
| Masculine | 28 | 46,6% | |
| Origin | |||
| Lambayeque | 54 | 90,0% | |
| Other | 6 | 10,0% | |
| Educational level | |||
| Complete high school | 16 | 26,6% | |
| Institute | 13 | 21,6% | |
| Incomplete high school | 10 | 16,6% | |
| University | 7 | 11,6% | |
| Complete grade school | 4 | 6,6% | |
| Incomplete grade school | 3 | 5,0% | |
| Incomplete higher education | 6 | 10,0% | |
| Illiterate | 1 | 1,6% | |
| Diagnosis | |||
| Schizophrenia | 21 | 35,0% | |
| Mild mental retardation | 4 | 6,6% | |
| Bipolar disorder | 5 | 8,3% | |
| Borderline personality disorder | 3 | 5,0% | |
| Depression dissocial disorder | 3 | 5,0% | |
| Recurrent depressive syndrome | 3 | 5,0% | |
| Other | 21 | 35,0% | |
| Occupation | |||
| Unemployed | 46 | 76,6% | |
| Employed | |||
| Trade | 11 | 18,3% | |
| Professional | 3 | 5,0% | |
| Marital Status | |||
| Single | 38 | 63,3% | |
| Married | 12 | 20,0% | |
| Others | 10 | 16,6% | |
The median of hospitalization time was 12.5 days (RIC: 8-17,7 days). Of the 60 patients, the questions that obtained greater rates were the following: for the category “a lot or very much” the questions “How much would it matter to you to embarrass your family?” (43/60), “How proud are you of your family?” (33/60), for the category “none or a little” the question “Do you feel you can count on your family when you have problems?” (22/60), and for the category “regular’ the question “How much do you feel you support one another?” (27/60) (seeTable 2).
Table 2. Questions linked to family cohesion in the psychiatric patient treated in H.A.A.A.
| Questions | Nothing or little | Regular | A lot or very much |
|---|---|---|---|
| How much would it matter to you to embarrass your family? | 6 (1%) | 11 (18,3%) | 43 (71,7 %) |
| How much do you feel respected? | 17 (28,3%) | 25 (41,6%) | 18 (30%) |
| How much do you feel you support one another? | 10 (16,6%) | 27 (45%) | 23 (38,3%) |
| How proud are you of your family? | 8 (13,3%) | 19 (31,6%) | 33 (55%) |
| How much do you feel your values are similar to those of your family? | 14 (23,3%) | 24(40%) | 22(36,6%) |
| How much do you feel part of the progress of your family? | 19 (31,6%) | 23 (38,3%) | 18 (30%) |
| Do you feel you can count on your family when you have problems? | 22 (36,6%) | 15 (25%) | 23 (38,3%) |
| Do you discuss your personal issues with your family? | 20 (33,3%) | 22 (35,6%) | 18 (30%) |
| Do they take your opinion into account in important decisions? | 16 (26,6%) | 23 (38,3%) | 21 (35%) |
| Does your family show interest in your feelings? | 14 (23,3%) | 23 (38,3%) | 23 (38,3%) |
| Do you feel your family takes you into account? | 14 (23,3%) | 20 (33,3%) | 26(43,3%) |
Regarding the days of hospitalization for the questions related to family cohesion, the questions that had a higher median of hospitalization days for those that responded, “nothing or little” were the following questions: “How much would it matter to you to embarrass your family?” and “How proud are you of your family?” with a median of 15 days and of 15.5 days, respectively (Table 3).
Table 3. Hospitalization time based on questions related to family cohesion of psychiatric patients from Hospital Almanzor Aguinaga Asenjo.
| Questions | Nothing or little | Regular | A lot or very much | |||
|---|---|---|---|---|---|---|
| Median | R.I | Median | R.I | Median | R.I | |
| How much would it matter to you to embarrass your family? | 15 | 12 - 26,25 | 10 | 6 - 24 | 12 | 8 - 18 |
| How much do you feel respected? | 12 | 8 - 17 | 15 | 7 - 19,5 | 12,5 | 7,75 - 18,25 |
| How much do you feel you support one another? | 12 | 8,5 - 20 | 15 | 9 - 18 | 12 | 7 - 18 |
| How proud are you of your family? | 15,5 | 10,5 - 31,75 | 10 | 6- 19 | 13 | 8 - 17 |
| How much do you feel your values are similar to those of your family? | 10 | 8,5 - 18,75 | 14 | 6 - 18 | 14 | 8,75 - 19 |
| How much do you feel part of the progress of your family? | 10 | 7 - 17 | 17 | 8 - 24 | 15 | 7,75 - 17,25 |
| Do you feel you can count on your family when you have problems? | 10 | 6,75 - 17,75 | 12 | 8 - 17 | 15 | 9 - 19 |
| Do you discuss your personal issues with your family? | 10 | 5 - 19,25 | 14,5 | 8 - 17,25 | 14,5 | 11 - 21,5 |
| Do they take your opinion into account in important decisions? | 9,5 | 6 - 16,25 | 15 | 8 - 17 | 15 | 8,5 - 19 |
| Does your family show interest in your feelings? | 12 | 8,5 - 17, 75 | 12 | 6- 19 | 14 | 8 - 18 |
| Do you feel your family takes you into account? | 12 | 7 - 17,75 | 13,5 | 6- 19 | 14,5 | 8 - 18 |
For those who responded “a lot or very much”, the questions with a higher median of hospitalization days were the following questions: “Do you feel you can count on your family when you have problems?”, “Do they take your opinion into account in important decisions?” and “Do you feel your family takes you into account?” with a median of 15 years and 14.5 days for the first two and for the last one, respectively (Table 3).
DISCUSSION
In the studied population, the median age was 50 years of age, the female gender predominated slightly (53%), and the most frequent diagnosis was schizophrenia (35%). The average age of the studied population was 50 years, which differs from other studies where the average age was of young adults (20 -40 years) (3,8. Likewise, the male gender predominated in the majority of studies3,8. As far as similarities to other studies, the most frequent diagnosis was schizophrenia3,8. We researched that having a psychiatric disorder potentially affected personal achievement9, which could be why the majority of patients in the current study were single, unemployed and without higher education. The median hospitalization days in this study was 12.5 days, which is much less in comparison to the hospitalization time of other studies whose average was 21 days(10). This could be because during hospitalization the focus is directed towards stabilizing acute mental disorder symptoms and not towards a strict control of the disease during hospital stay, such as the medical treatment follow-up after compensating the crisis and educating family members as a primary source of support to lower patient relapse(11). Also, having been one of the only hospitals that has exclusive hospitalization for psychiatric patients they avoid inappropriately occupying hospital beds, which could generate pressure for an early discharge11. Early diagnosis may also influence prolonged hospitalizations4since not all have the same severity, however, it is ruled out that disease type may influence that hospitalization days be shorter here than in other hospitals, since in the majority of studies schizophrenia diagnosis was prevalent just as in this study3,8,9. We found that in two questions when patients responded in a positive manner, they had lower hospital stay. 72% (43/60) of patients cared “a lot or very much” about embarrassing their family, and 55% of patients felt proud of their family: in both questions they had less hospitalization days in comparison to those who responded, “little or none”. Patients with psychiatric disorders feel and live their condition, which causes them to feel blame, fear and shame for their attitude due to society stereotypes and prejudice12. These feelings reflect in their interaction with society and how it affects their families’ feelings. In the same manner, the majority of patients feel that their family does not respect them. We found that 42% of patients feel that their family respects them in a regular manner, while 28% feel that they do not respect them. In this respect we take into account that anyone with any psychiatric disorder is considered different in society, violating ethical principles that prevent them from being treated with the respect they deserve13. Patients with interfamily support, who count on family in case they have problems and feel that they are taken into account, remained hospitalized longer. Different studies reveal that counting on support is an important factor for the progress of disease and less hospitalization days in a patient with a psychiatric disorder since the family’s attitude with respect to the disorder of one of its family members is vital for their treatment and recovery9. However, hospitalization days are more prolonged in patients who count on family support than in those who responded “none or little” to the questions in the survey questionnaire. These results may be influenced by the distortion of reality in schizophrenic patients, in whom their distorted perception leads them to assert that they do not have a mental disorder or any problem in their lives(14) As a limitation, despite the questionnaire used is an instrument used and adapted by the Instituto Nacional de Salud Mental Hideyo Noguchi, we were no table to determine if the patient has family cohesion or not, discussing the questions separately. However, the study’s importance is highlighted for having served as a first step to evaluate how much support psychiatric patients receive from their families and exposes the need to count on an instrument to evaluate family cohesion from the patient and from the family member in charge.
CONCLUSION
The age median was 50 years, the female gender slightly predominated, and the most frequent diagnosis was schizophrenia. The hospitalization time (12.5 days) was much lower than the average time in other studies and it did not meet the psychiatric service minimum of 60 days, an established norm under the general mental health law in Peru. The majority of patients cared about embarrassing their family and felt proud of it. Those who responded questions in a positive manner, tended to remain hospitalized longer than those who responded negatively. We suggest developing an instrument to evaluate family cohesion, from the patent as well as from the family member in charge of their care, one that may be taken as a reference for future research considering the lack of studies in this topic.
REFERENCES
1. Morro Fernández L. Factores sociofamiliares y estancia hospitalaria: la complejidad de la intervención social en el área de la psiquiatría de agudos. Aplicación de la escala ECISACH-BCN PSMAR. Altern Cuad Trab Soc. 2017;1(24):137-60. DOI: https://doi.org/10.14198/ALTERN2017.24.08. [ Links ]
2. Ruiz E. Factores asociados a la estancia prolongada en el Servicio de Medicina Internal Hospital Nacional Arzobispo Loayza 2016. [Internet] [Tesis de grado] [Lima]: Universidad San Martín de Porres; 2016. Disponible en: http://repositorio.usmp.edu.pe/bitstream/handle/20.500.12727/2610/RUIZ_ER.pdf?sequence=1&isAllowed=y [ Links ]
3. Pérez JJN, Marqués ÁC. Sobrecarga familiar, apoyo social y salud comunitaria en cuidadores de personas con trastorno mental grave. Rev da Esc Enferm da USP. 2018;52:1-8. DOI: https://doi.org/10.1590/s1980-220x2017029403351 [ Links ]
4. Cubero M, Castillo M. Calidad de vida de pacientes esquizofrénicos según su percepción. [Internet] [Tesis de grado] [Ecuador] Universidad del Azuay; 2016. Disponible en: http://dspace.uazuay.edu.ec/handle/datos/4994 [ Links ]
5. Chero D, Cabanillas A. Características de los pacientes adultos con estancia prolongada atendidos en el servicio de emergencia en el Hospital Base Almanzor Aguinaga Asenjo (HBAAA) durante los meses de febrero y marzo del año 2016. [Internet] [Tesis de grado] [Chiclayo, Perú] Universidad Católica Santo Toribio de Mogrovejo; 2016. Disponible en: http://tesis.usat.edu.pe/bitstream/20.500.12423/1009/3/TL_CabanillasOlivaresAngella_CheroFarroDialy.pdf [ Links ]
6. Perales A, Sogi C, Salas RE. Salud Mental en adolescentes del distrito de Magdalena. En Serie: Monografías de Investigación Nro. 4. Lima: INSM "Honorio Delgado-Hideyo Noguchi". An Salud Ment. 1996;18:1-200. [ Links ]
7. Arellano M., Bernal E., Chuchón V., Cutipé Y., Gonzáles S., Márquez S. et al. Confiabilidad y Validez de los cuestionarios de los Estudios Epidemiológicos de Salud Mental de Lima y de la Selva Peruana. Rev An SALUD Ment.[Internet] julio de 2016 [Citado 24 de Enero del 2021];25(1). Disponible en: http://www.insm.gob.pe/investigacion/archivos/estudios/2009-ASM-CVCEESMLSP/files/res/downloads/book.pdf [ Links ]
8. Abanto R, Valdivieso-Jiménez G, Arévalo A, Orihuela S. Características personales, clínicas y sociales en pacientes con estancia hospitalaria prolongada en los pabellones de pacientes agudos del Hospital Víctor Larco Herrera. Horiz Médico. diciembre de 2018;18(2):60-70. DOI: http://dx.doi.org/10.24265/horizmed.2018.v18n2.10. [ Links ]
9. Cristian Guaitero, Guaranguay J. Calidad de vida de pacientes con enfermedad mental en una IPS de la ciudad de Bogotá. [Internet] [Tesis de grado] [Colombia] Universidad de Ciencias Aplicadas y Ambientales; 2018. Disponible en: https://repository.udca.edu.co/handle/11158/1179 [ Links ]
10. Osorio M JP, Parrini V J, Galdames G F, Dinamarca C F. Length of stay in psychiatric hospitalization in patients with GES diagnoses and its comorbidities. Rev Chil Neuropsiquiatr. marzo de 2016;54(1):19-26. DOI: http://dx.doi.org/10.4067/S0717-92272016000100003. [ Links ]
11. Dimitri G, Giacco D, Bauer M, Bird VJ, Greenberg L, Lasalvia A, et al. Predictors of length of stay in psychiatric inpatient units: Does their effect vary across countries? European Psychiatry. febrero de 2018;48(1):6-12. DOI: 10.1016/j.eurpsy.2017.11.001 [ Links ]
12. Márquez HMP, Trejo GJ, Estupiñán MFV. Medición del estigma internalizado y su relación con la adaptación social en pacientes psiquiátricos. Rev Esp Cienc Salud. 2012;15(2):88-92. Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=42724 [ Links ]
13. Loubat M, Lobos R, Carrasco N. Estigmatización de la persona con esquizofrenia y consecuencias para el proyecto de rehabilitación. Revista Interdisciplinaria de Filosofía y Psicología. 2017;12(39):15-25. Disponible en; https://www.revistalimite.cl/index.php/limite/article/view/75 [ Links ]
14. Figueroa A, Durán E, Mendizábal N, Oyarzún S. El juicio de realidad y mundos posibles en personas con esquizofrenia. Rev Chil Neuropsiquiatr. 2017;55(3):195-204. DOI: http://dx.doi.org/10.4067/s0717-92272017000300195 [ Links ]
Received: October 29, 2020; Accepted: January 24, 2021











 texto en
texto en