Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista de la Facultad de Medicina Humana
versão impressa ISSN 1814-5469versão On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.21 no.3 Lima jul./set. 2021
http://dx.doi.org/10.25176/rfmh.v21i3.3942
Clinical case
Autologous serum in vascular ulcer of long evolution
1. Instituto de investigación de ciencias biomédicas INICIB, Facultad de Medicina Humana, Universidad Ricardo Palma
2. Instituto Peruano de Ingeniería Celular y Manufactura de tejidos INGECEL
The treatment of chronic wounds continues to be a topic of great interest due to its slow evolution and difficult healing, despite the development of new therapies on wound care and treatment. We present the case of a 76-year-old male patient with a 3-year-old chronic vascular ulcer located in the distal portion of the left leg, with severe incompetence of the small saphenous vein predominantly in the left lower limb. The application of autologous serum is proposed as an alternative treatment, managing to reactivate the repair process and subsequent wound healing, which was not achieved with conventional treatment.
Keywords: Autologous serum; Vascular ulcers; Scarring (fuente: MeSH NLM).
INTRODUCTION
The treatment of chronic wounds continues to be a topic of great interest, despite the development of new therapies for the care and management of wounds that are difficult to resolve, due to the slow or prolonged injuries healing evolution.
Lesions of vascular origin are generally associated with diabetic patients, who usually have a recurrence up to five years in 70% of cases1. It represents an important cause of morbidity in the world due to its tendency to chronicity, even reaching the amputation of the limb.
Vascular lesions in non-diabetic patients, characterized by significant alterations in the peripheral and deep blood circulation, also represent a serious problem due to their predisposition to infections, which is related to the severity of the ulcer2. This situation leads to recurrent hospitalizations, and in some cases long periods of absence from work, which entails high costs for hospital economic costs and have a direct impact on quality of life3.
A series of studies have been carried out on growth factors, achieving a certain consensus on the benefit they provide by efficiently reducing repair time and wound healing2.
However, questions arise in the medical community about how to predict the proper ratio between the different factors involved in the repair process. Currently, some growth factors have been isolated, but these are not yet available to the entire population, unlike autologous serum2.
In this clinical case, the autologous serum obtained from whole blood with calcium citrate was used, which was centrifuged at 3,500 rpm in 8 minutes and all of the autologous serum was separated. This was activated with 10% calcium chloride, and covered with paraffin gauze dressing and gauze. This protocol was repeated with intervals of 4 days4.
The application shows an activation of the initial healing within the first 24 hours, where it is observed how the dermal buttons begin to be stimulated, which are replacing the initial scar tissue by noble tissue.
CLINICAL CASE
A 76-year-old male patient, retired, from Huari (home town) and Lima. As a pathological history, he presented a left hip prosthesis due to osteoarthritis, with a 10-year evolution time. His disease began 3 years ago, initially presenting a dermal lesion type phlyctena in the internal malleolus of the left foot. It went through intermittent stages of exacerbation, modifying its appearance and size, with an intermittent positive response to clinical management of antibiotic therapy (oral route) and topical treatment (regenerative creams). On occasions, hospitalization was carried out to expand the study of the patient, clinical management, and antibiotic therapy (intravenously), performing daily cures with biological dressings to control the extent of the lesion.
He arrives at our service, presenting an injury in the distal region of his left leg. Oral antibiotic management was performed with ciprofloxacin 500mg every 12 hours and paracetamol 500mg every eight hours, but without apparent improvement during the last month. (View photos).
Physical examination revealed a lesion measuring approximately 10x15 cm, extending from the medial malleolus to the external malleolus in a surrounding manner. It is covered with a hydrocolloid dressing, with 80% granulation tissue, serohematic secretion, signs of maceration and foul odor, irregular borders, erythema and surrounding edema. Distal pulse present and pain of 5/10 according to visual analogue scale.
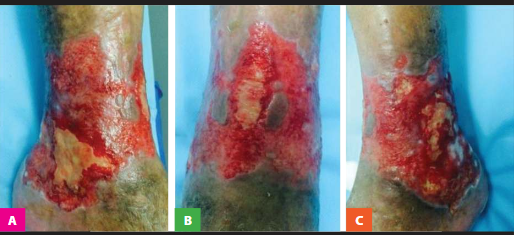
Figure 1: A) View of the inner of the left leg B) Anterior view of the distal portion of the left leg, and C) View of the outer of the left leg
In auxiliary examination: hemoglobin of 13 mg/dL, sedimentation rate of 20 mm/h, C-reactive protein of 1.76 mg/L, glucose 105 mg/dL, creatinine 1.60 mg/dL. Secretion culture of the sample positive to S. aureus, resistant to ciprofloxacin and sensitive to clindamycin.
Treatment with clindamycin 300 mg every eight hours is started and a first cleaning of the affected area was performed with Isodine foam and solution, Later sodium chloride is applied to the bloody bed, it is covered with autologous serum gauze topically and paraffin gauze; occlusive closure is performed for 24 hours.
At 24 hours, the occlusive patch was opened and a reduction of the bloody bed was evidenced, areas with the presence of macerated tissue and a velvety appearance, with the appearance of dermal buttons (view photo).

Figure 2: 24 hours after starting therapy, where an immediate response to the initial healing process is observed. A) View of the inner of the left leg B) Anterior view of the distal portion of the left leg, and C) View of the outer of the left leg

Figure 3: Photograph 48 hours after starting therapy, where a reduction of the affected area is appreciated, with decreased secretion, erythema and surrounding edema.

Figure 4: Photograph of the initial healing progress 7 days after starting the treatment, where residual areas of lesion in progress of resolution can be seen, with epithelialization areas
The lesion progresses favorably until the 4th week, obtaining 95% healing and leaving a residual lesion in the internal malleolus region with characteristics similar to those described in the initial process 3 years ago, without further progress.
A venous Doppler exam was performed, finding severe incompetence of the small saphenous vein, with slight incompetence of the distal great saphenous vein, perforating and accessory veins. We proceeded to the specialist to perform a surgical correction of the vascular lesion.
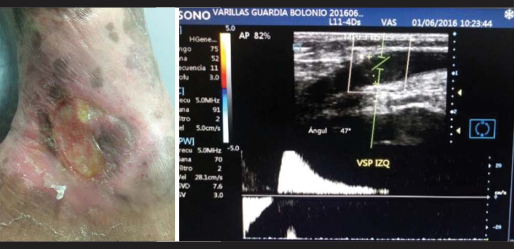
Figure 5: Residual lesion in the internal malleolus of the left leg. Doppler ultrasound showing incompetence of the small saphenous vein, with slight incompetence of the distal great saphenous vein, perforating and accessory veins
A total closure of the lesion is achieved after 3 months from the start of treatment with the autologous serum.
DISCUSSION
Chronic vascular lesions become a vicious circle due to their ease of contamination, a process characterized by an excessive increase in the production of pro-inflammatory cytokines and proteolytic enzymes. This causes an alteration in the pH of the affected area, making the repair and healing process difficult.
In general, patients with chronic vascular lesions are usually cared for in a conventional way, receiving antibiotic/antimicrobial treatment for 2 weeks, daily topical dressings and covered with hydrogels or foams that allow exudate control until the elimination of the infection, improving the conditions of injury.
Autologous serum is used as an alternative therapy in the absence of response to conventional treatment, in order to help restore the inactivity of growth factors5. This massive release of proteins 5-8 times their physiological concentration, secreted by platelets, exerts its action to promote repair5.
Monton E, et al., presented a retrospective study of clinical practice (vascular ulcers, diabetic feet, radiopathies, loss of substance, complex cases and reconstruction). In this study, 151 patients were evaluated, of whom 47 received another type of treatment for a period of 30 months, using platelet-rich plasma (PRP) in chronic wounds with 6 months of treatment6. A significant, although not significant, reduction in the time to healing was obtained in patients treated with PRP (mean 2.6 months) compared to the previous time (11.9 months). This improvement was achieved in 72% of the patients (n = 108) through a single application of PRP, alone or in combination6.
Several cases were reported where the evolution of reparative phenomena were absent or appeared for very long periods of time (23 years in one reported case), and in which multiple reparative procedures had failed. Very favorable results were obtained from the point of view of the efficacy of cures after therapies based on clinical observation of the evolution of the reparative process6.
The use of autologous serum is a therapy that is increasingly used in clinical practice in different specialties due to the benefits it provides in accelerating tissue repair processes. To date, no adverse reactions have been reported; this probably because it is easy to extract and manipulate under established protocols. In addition, it is a therapy that reduces hospital costs that usually cause this type of chronic injury.
REFERENCES
1. J.S. López García, I. García-Lozano, J. Martínez-Garchitorena. Aplicaciones del suero autólogo en oftalmología. Arch Soc Esp Oftalmol, 82 (2007), pp. 9-20 https://doi.org/10.4321/s0365-66912007000100004 [ Links ]
2. E. Grynberg Laloum, P. Senet. Ulceras de la pierna. EMC - Tratado de Medicina. 2015:19(2);1-10. https://doi.org/10.1016/S1636-5410(15)70943-8 [ Links ]
3. J. Esquirol Caussa, E. Herrero Vila. Un enfoque del Tratamiento de las ulceras de origen vascular: revisión y papel del factor de crecimiento epidérmico. Angiología . 2016:68(4);322-330. https://doi.org/10.1016/j.angio.2015.10.002 [ Links ]
4. S.A. Bus, J.J. van Netten, L.A. Lavery, M. Monteiro-Soares. IWGDF guidance on the prevention of foot ulcers in at-risk patients with diabetes. Diabetes Metabolism Research and Reviews. 2016:32(S1);16-24 https://doi.org/10.1002/dmrr.2696 [ Links ]
5. Rossani G.,Hernandez I., Alcolea J.M., Castro Sierra R., Perez Soto W., TrellesM., Tratamiento de Quemaduras mediante plasma rico en plaquetas (Prp). Cir.Plast.Iberolatinoam. 2014:40(2);229-238. http://dx.doi.org/10.4321/S0376-78922014000200015 [ Links ]
6. Carrasco J, Bonete D, Gomar F. Plasma rico en plaquetas vs. plasma rico en factores de crecimiento. Revista Española de Cirugía Osteoarticular. 2009; 239: 127-137. https://www.google.com.pe/url?sa=t&rct=j&q=&esrc=s&source=web&cd=2& cad=rja&uact=8&ved=2ahUKEwjk3YzSi8HiAhXMxVkKHcoqDdUQFjABegQI ABAB&url=http%3A%2F%2Fscielo.isciii.es%2Fscielo.php%3Fscript%3Dsci _abstract%26pid%3DS1130- 05582006000200001&usg=AOvVaw15cxoCeSWcslwW97BCRU5r [ Links ]
7. Montón Echeverria J., Pérez Redondo S., Gómez Bajo G. Experiencia clínica en el empleo de factores de crecimiento autologos, obtenidos de plasma rico en plaquetas. Cir. Plast. iberolatinoam. 2007; 33 (3):155. https://www.google.com.pe/url?sa=t&rct=j&q=&esrc=s&source=web& cd=1&ved=2ahUKEwj5g9vHisHiAhWjwFkKHaAPB9wQFjAAegQIBRA C&url=http%3A%2F%2Fscielo.isciii.es%2Fpdf%2Fcpil%2Fv33n3%2F 155.pdf&usg=AOvVaw0vpv-IEgRCpbtGlLX9cAGI [ Links ]
Received: May 25, 2021; Accepted: June 16, 2021











 texto em
texto em 



