Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista de la Facultad de Medicina Humana
versão impressa ISSN 1814-5469versão On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.21 no.4 Lima out./dez. 2021
http://dx.doi.org/10.25176/rfmh.v21i4.3902
Clinical case
Posner - Schlossman syndrome: Case report
1Hospital Nacional Carlos Alberto Seguín Escobedo - EsSalud. Arequipa, Peru.
2Universidad Nacional de San Agustín. Medical school, Arequipa, Peru.
3Universidad Nacional Mayor de San Marcos. Medical school, Lima, Peru.
Introduction:
Posner - Schlossman Syndrome (PSS) is a rare disease, more prevalent in men between 20 and 50 years old, characterized by recurrent attacks of anterior uveitis and ocular hypertension.
Clinical case:
We report the case of a 42-year-old patient with a single eye. He came to the consultation presenting decreased visual acuity, photobobia, halos around the lights, and intense pain in his left eye. The ophthalmological examination revealed inflammatory signs in the anterior segment, elevated intraocular pressure and damage to the optic nerve. Medical treatment was started with corticosteroids and topical antiglaucoma drugs, oral acetazolamide and intravenous mannitol, obtaining no response and it was decided to perform a surgical intervention (Ahmed valve implantation) in the left eye, subsequently achieving a good clinical evolution and resolution of the case.
Conclusion:
This report highlights that the episodic and recurrent nature of SPS requires strict monitoring.
Keywords: Posner-Schlossman syndrome; anterior uveitis; ocular hypertension (Source: MeSH NLM).
INTRODUCTION
Posner-Schlossman Syndrome (PSS) or glaucomatocyclitic crisis is a rare disease characterized by recurrent attacks of non-granulomatous anterior uveitis and elevated intraocular pressure (IOP) (ocular hypertension). This is frequently classified as a secondary inflammatory glaucoma1,2,3.
PSS main clinical manifestations are elevated IOP and blurred vision, tending to affect patients between 20 and 50 years old, most often men than women. The episodes are unilateral, although in 50% of patients the other eye is involved at some point. Intervals between attacks vary, but usually lengthen over time1,4.
The etiology of PSS has been investigated in some studies, which indicated that PSS may be associated with cytomegalovirus (CMV) infection, genetic susceptibility, inflammatory cytokines, and vascular endothelial dysfunction. Among these, CMV infection is considered a vital risk factor for PSS5,6.
PSS diagnosis is inherently difficult. The subtlety of some features of low-grade anterior uveitis and the short-lived nature of each attack makes it hard to diagnose. PSS must be differentiated from acute angle-closure glaucoma, primary open-angle glaucoma, uveitic glaucoma, and Fuchs heterochromic iridocyclitis7.
Treatment for PSS is aimed at controlling inflammation and elevated IOP. However, some patients do not respond to corticosteroids or antiglaucoma medications. In these cases, surgery is needed to lower the IOP and thus prevent the visual field defects progression and damage to the optic nerve3,8.
This case refers to a patient with a history of SPS attacks, who initially received maximum anti-inflammatory and anti-glaucoma medical treatment, but as there was no response, surgical treatment was required.
Clinical case
We present the case of a 42-year-old man who presented with decreased visual acuity, photophobia, halos around lights, and severe pain in his left eye (LE) for 5 days. The patient refers that these symptoms have been presenting for 4 years in a mild and transitory way, so he has not required medication.
As an ophthalmological history, the patient underwent surgery for ocular trauma in the right eye (RE) approximately 30 years ago, with poor subsequent evolution. At ophthalmological examination, he presents a corrected visual acuity of no light perception in RE and 20/70 in LE. IOP was 15 mmHg in the RE and 50 mmHg in the LE. In the anterior segment examination with a slit lamp in the RE, an extensive corneal opacity of central predominance of whitish-gray appearance with stromal deposits was evidenced, which did not allow to see other details of the anterior segment; n the LE, mild corneal edema was evidenced, with the presence of fine keratic precipitates in the middle third and lower 1/3 of the corneal endothelium, no atrophy or heterochromia of the iris, anterior chamber reaction: Tyndall and Flare (1+), wide anterior chamber, lens opacity NO1 NC1 C2 P1, 360 ° cilium-conjunctival injection (Figure 1). At gonioscopy, the RE could not be evaluated due to corneal opacity, the LE showed an open angle (Shaffer grade IV). In the fundus examination, the RE could not be evaluated due to the opacity of the media, in the LE a papilla with defined edges was evidenced, excavation of 0.4, with nasal rejection of the central vessels, with preserved macular shine, without inflammation signs in the posterior segment (Figure 2).
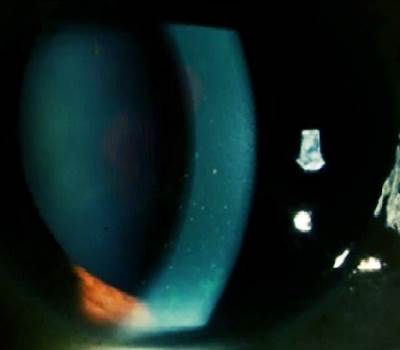
Figure 1: Slit lamp examination reveals fine keratic precipitates in the middle third and lower 1/3 of the corneal endothelium of the LE. (Source: Medical history)
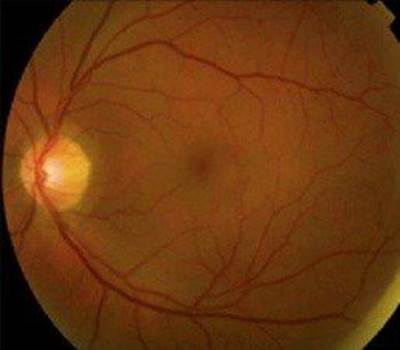
Figure 2: The fundus examination reveals a papilla with defined edges, a 0.4 excavation, with nasal rejection of the central vessels. (Source: Medical history)
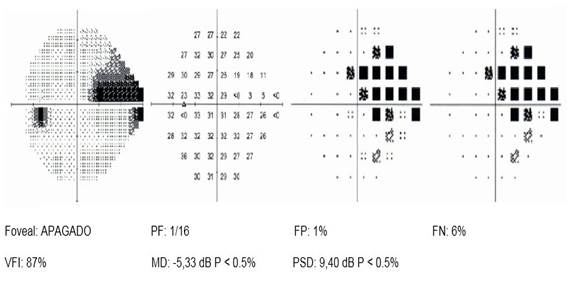
Visual field exploration was performed with program 24-2 of the Humphrey visual field analyzer, which revealed the presence of a nasal step in the LE (Figure 3).
Laboratory tests were requested: complete blood count (CBC), acute phase reactants, antinuclear antibodies, rheumatoid factor, toxoplasmosis serology, serology for cytomegalovirus, serology for syphilis, serology for HIV, serology for HTLV 1 and 2, serology for hepatitis, all of which were normal.
Due to all the above, the diagnosis of Posner-Schlossman syndrome is made and medical treatment with Acetazolamide (250mg) is started. 1 tablet every 8 hours, Brimonidine (0.2%) 1 drop every 12 hours, Dorzolamide (2%) 1 drop every 8 hours, Timolol (0.5%) 1 drop every 12 hours and Prednisolone (1%) 1 drop every 4 hours in the LE. It was reassessed 48 hours after starting the medical treatment, the patient reported that the symptoms had not improved, the decrease in IOP to 40 mmHg and the persistence of inflammatory signs in the anterior segment of the LE. Mannitol (20%) 250 ml is added every 8 hours intravenously. A new evaluation is carried out 5 days after starting medical treatment and a decrease in IOP to 30 mmHg in LE is observed, therefore it is evident that there was not an adequate response to maximum medical treatment.
Faced with this situation, it was decided to place a drainage device and extract the cataract from the LE. Surgical treatment is performed by implanting the Ahmed valve, phacoemulsification, and placement of an intraocular lens in LE
In the postoperative period, the IOP was normal, without any pharmacological medication. A week after surgical treatment, a visual acuity of 20/25 was obtained with correctors and an IOP of 10 mmHg with clinical relief of ocular symptoms in the LE.
The follow-up was carried out initially once a week, then monthly, IOP remained normal without any pharmacological medication for more than 6 months after surgery, without attacks of PSS.
DISCUSSION
Posner - Schlossman syndrome is a rare disorder, a form of anterior uveitis with ocular hypertension and a higher prevalence in men between 20 and 50 years old9, characteristics that correspond to our patient, who was 42 years old and presented the characteristic clinical picture of this disease.
Posner-Schlossman syndrome has some clinical features of glaucoma and uveitis, such as ocular hypertension and the presence of retrokeratic precipitates10. These inflammatory signs (retrokeratic precipitates and reaction in the anterior chamber) and the markedly elevated intraocular pressure were described in the initial clinical picture presentation in our patient.
Early diagnosis and proper treatment may lower the risk of advanced glaucoma. Frequent attacks of ocular hypertension are particularly dangerous because they can easily affect vision by causing progressive visual field defects. Therefore, IOP control is the most important goal of treatment1,10.
Initial treatment for PSS is a combination regimen of anti-inflammatory and anti-glaucoma drugs. A topical corticosteroid is often successful in controlling inflammation. Ocular hypertension usually normalizes with control of inflammation. Topical β-blockers and / or carbonic anhydrase inhibitors are the drugs of choice in patients with PSS. Prostaglandin analogs efficacy in PSS is not well established. α2-agonists may also represent a good therapeutic option. If PSS attacks show higher frequency and IOP fluctuations are significant with attacks, surgical intervention may be indicated10,11. The most commonly indicated technique is filtering surgery (Trabeculectomy), especially in patients with recurrent attacks and IOP peaks, with damage to the optic nerve and visual field defects12. Another technique also used is valve implant drainage device surgery, which in many studies is considered the preferred first-line surgery in the treatment of uveitic glaucomas13,14. Our patient received maximum medical treatment, which was insufficient for IOP control, so a surgical intervention was finally performed, placing a valved drainage device (Ahmed valve).
PSS is known as a self-limited ocular disease with benign prognosis, but glaucomatous deterioration of visual function in some patients is increasingly reported, therefore, early diagnosis and appropriate treatment of SPS could decrease the risk of progression to advanced glaucoma15,16.
CONCLUSIONS
Posner-Schlossman syndrome or glaucomatocyclitic crisis is a rare disease, characterized by recurrent attacks of anterior uveitis and ocular hypertension. PSS usually has a good response to medical treatment, but as observed in the present case, IOP could not be controlled, so a surgical intervention was required, achieving a good clinical evolution after this. The episodic and recurrent nature of PSS requires close monitoring, therefore, patients with SPS should have regular evaluation of visual acuity, visual field, and IOP.
REFERENCES
1. Yang MM, Sun HY, Meng T, et al. CFH I62V as a Putative Genetic Marker for Posner-Schlossman Syndrome. Front Immunol. 2021;12:1-9. DOI: 10.3389/fimmu.2021.608723 [ Links ]
2. Megaw R, Agarwal PK. Posner-Schlossman syndrome. Surv Ophthalmol. 2017;62:277-285. DOI: 10.1016/j.survophthal.2016.12.005 [ Links ]
3. Murata K, Ishida K, Ozawa K, et al. The characteristics of Posner-Schlossman syndrome: a comparison in the surgical outcome between cytomegalovirus-positive and cytomegalovirus-negative patients. Medicine. 2019;98:48:1-8. http://dx.doi.org/10.1097/MD.0000000000018123 [ Links ]
4. Salmon J. Kanski Oftalmología Clínica. Editorial Elsevier. 9° edición. 2019. [ Links ]
5. Su C-C, Hu F-R, Wang T-H, et al. Clinical outcomes in cytomegalovirus-positive Posner-Schlossman syndrome patients treated with topical ganciclovir therapy. Am J Ophthalmol. 2014;158:1024-1031. DOI: 10.1016/j.ajo.2014.08.007 [ Links ]
6. Zhai R, Wang Z, Sheng Q, et al. Polymorphisms of the cytomegalovirus glycoprotein B genotype in patients with Posner-Schlossman syndrome. Br J Ophthalmol. 2021;0:1-5. DOI:10.1136/bjophthalmol-2020-318284 [ Links ]
7. Green RJ. Posner-Schlossman syndrome (Glaucomatocyclitic crisis). Clin Exp Optom. 2007;90(1):53-56. DOI: 10.1111/j.1444-0938.2006.00088.x [ Links ]
8. Maruyama K, Maruyama Y, Sugita S, et al. Characteristics of cases needing advanced treatment for intractable Posner-Schlossman syndrome. BMC Ophthalmol. 2017;17(45):1-7. https://doi.org/10.1186/s12886-017-0438-y [ Links ]
9. Guo H, Zhang W, Ye Q. A meta-analysis of the rate and related factors of glaucomatous optic nerve damage in patients with Glaucomatocyclitic Crisis. Int Ophthalmol. 2020;40(11):3145-3153. https://doi.org/10.1007/s10792-020-01527-w [ Links ]
10. Shazly TA, Aljajeh M, Latina MA. Posner-Schlossman glaucomatocyclitic crisis. Semin Ophthalmol. 2011;26(4):282-284. DOI: 10.3109/08820538.2011.605821 [ Links ]
11. Lippert J, Falgiani M, Ganti L. Posner - Schlossman Syndrome. Cureus. 2020;12(1):1-5. DOI: 10.7759/cureus.6584 [ Links ]
12. Zhong Y, Cheng Y, Liu X, et al. Trabeculectomy in the Management of Glaucomatocyclitic Crisis with Visual Field Defect. Ocul Immunol Inflamm. 2010;18(3):233-236. DOI: 10.3109/09273940903499864 [ Links ]
13. Teoh SB, Thean L, Koay E. Cytomegalovirus in aetiology of Posner-Schlossman syndrome: evidence from quantitative polymerase chain reaction. Eye. 2005;19:1338-1340. https://doi.org/10.1038/sj.eye.6701757 [ Links ]
14. Muñoz F, Moreno J, Hernandez P, Rebolleda G. Current Approach in the Diagnosis and Management of Uveitic Glaucoma. Biomed Res Int. 2015;742792:1-13. http://dx.doi.org/10.1155/2015/742792 [ Links ]
15. Jap A, Sivakumar M, Chee SP. Is Posner-Schlossman syndrome benign?. Ophthalmol. 2001;108(5):913-918. DOI: 10.1016/s0161-6420(01)00551-6 [ Links ]
16. Tsai JC. Detection of progression of retinal nerve fiber layer loss by optical coherenc tomography in a patient with glaucomatocyclitic crisis. Taiwan J Ophthalmol. 2015;5(2):90-93. DOI: 10.1016/j.tjo.2014.12.001 [ Links ]
Received: May 15, 2021; Accepted: July 11, 2021











 texto em
texto em