Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista de la Facultad de Medicina Humana
versão impressa ISSN 1814-5469versão On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.21 no.4 Lima out./dez. 2021
http://dx.doi.org/10.25176/rfmh.v21i4.4041
Clinical case
Atrial fibrillation that required cardioversion in the post anesthetic recovery unit in ambulatory surgery. A case report
1Clínica Internacional, San Borja, Lima - Perú.
2Instituto Nacional Cardiovascular “Carlos Alberto Peschiera Carrillo” INCOR.
3Hospital Nacional Guillermo Almenara Irigoyen
In recent years, the profile of patients who can undergo ambulatory surgery procedures in independent ambulatory surgical centers has changed. It is very important to consider the availability, skills and experience of the care staff, as well as the integral study of the patient, the resolution capacity of these centers and evaluations with quality care indicators to obtain optimal results. The present case was of a 34-year-old male, first presentation of rapid and symptomatic atrial fibrillation documented in the immediate postoperative period. Patient care, diagnostic strategy and treatment were described, since the patient required electrical cardioversion.
Keywords: Atrial fibrillation; electrical cardioversion; otorhinolaryngology surgery; outpatient surgery (Source: MeSH NLM).
INTRODUCTION
Outpatient surgery is a modern, comfortable, safe, innovative and economical procedure that allows the patient to quickly and effectively resolve a surgical inconvenience and return home the same day of surgery. 70-80%1of medium and low complexity surgical procedures can be solved in ambulatory surgery centers,1thus avoiding nosocomial exposure, achieving resource optimization (cost reduction by up to 40%), reducing bed occupancy. However, patients who undergo surgery with greater comorbidities are more frequent. Unexpected adverse events may occur in young patients, such as this clinical case where the patient developed atrial fibrillation, half an hour after his stay in the post-anesthetic recovery unit. This case occurred in Clínica Internacional in Lima-Peru.
Clinical case
34-year-old male, mixed race, from the city of Lima, with fibromyalgia history, allergic rhinitis, undergoing rhinoplasty at 17 years of age, with a diagnosis of secondary septal deviation, left valve collapse and hypertrophy of inferior turbinates, which was scheduled for otorhinolaryngology surgery: ablusive septoplasty, plus bilateral turbinectomy with valvuloplasty. The patient received total intravenous general anesthesia (propofol and remifentanil), TIVA-TCI (total intravenous anesthesia-target control, infusion - goal-controlled anesthesia).
Clinical picture: Patient who in the Post-anesthetic Recovery Unit presented anxiety, referred dyspnea, tachycardic palpitations.
Malampatti I airway exam, good oral opening and cervical mobility, thyromental distance, grade I and Class I bite test.
Physical Exam: Pale skin and mucous membranes, devices and systems within normal limits.
Laboratory exams:
Hb15mmHg, Htco 45, leukocytes 4870, platelets 248,000, Group A +, TC 7, 'TS 2,' Glucose 93mmHg, Urea 29, Cr 0.9, Serological negative.
ASA II, Surgical Risk I, elective surgery.
During the intraoperative period, it is monitored with a 5-lead ECG (electrocardiogram), non-invasive blood pressure, oxygen saturation, capnography and monitoring of anesthetic depth, with the index qCon values 40-60 and the nocioceptive stimulus with the qNox values 40-60.
A surgical checklist is performed, pre-oxygenation is carried out, objective-guided total intravenous anesthesia was used, anesthetic induction was with Remifentanil 4ug./ml, propofol 2.5 ug./ml., With the mathematical models: MINTO for remifentanil and Marsh for Propofol, neuromuscular relaxation was with Rocuronium 0.6 mg./Kg., in the maintenance of anesthesia Propofol and remifentanil were used, according to site-effect objectives, cerebral anesthetic depth monitoring and non-invasive hemodynamic monitoring. Controlled mechanical ventilation parameters were carried out according to institutional protocols. The surgeon infiltrated lidocaine / adrenaline in the surgical area, showing no arrhythmias. During the surgery he was hemodynamically stable, he did not register cardiac arrhythmias, the surgical time was 2 hours 10 minutes.
As final analgesics he received Paracetamol 1gr. and tramadol hydrochloride 1-2mg / Kg. The surgical anesthetic act proceeds without complications, the patient is extubated and for reversal of neuromuscular relaxation, sugammadex 2mg / Kg is placed. The patient is taken to the Post-anesthetic Recovery Unit awake, calm, with stable vital functions, painless and collaborative.
In the immediate postoperative period, approximately half an hour after his stay in recovery, the patient suddenly becomes anxious, referring to dyspnea, tachycardial palpitations, without hemodynamic decompensation. The cardiac monitor showed supraventricular tachycardia, an irregular pulse of 143-160 bpm. A 12-lead electrocardiogram was performed and a cardiological evaluation was requested. Transthoracic echocardiography showed normal structures, preserved left ventricular function, and no intracavitary thrombi.
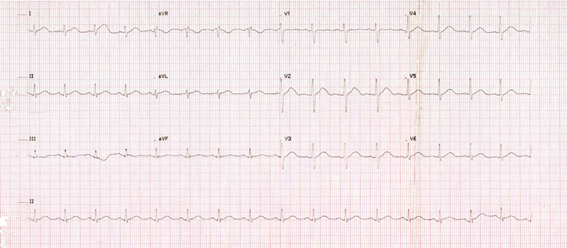
An anxious patient, as the palpitations were not self-limited and the irregular narrow QRS tachycardia persisted, amiodarone was indicated with a 300mg loading dose. and in infusion 600mg. After 2 hours of observation, Atrial Fibrillation persisted with high ventricular responseFig. 1, due to increased dyspnea and hemodynamic decompensation, it was decided to perform cardioversion under sedationFig. 2.
Electrical cardioversion vital functions Fc: 145 -160 x, ’PA: 80/60, SatO297%. Propofol 1 mg / kg was used as anesthetic, 150 joule was discharged, leaving sinus rhythm with the first discharge, the patient remains in the recovery unit for three more hours and is discharged for control by the cardiology office and treatment with propofenone 150mg c / 12 x 1 month.
Thus, care with effective electrical cardioversion is concluded. Procedure without complications, anticoagulation was not indicated, due to a greater risk of immediate postoperative bleeding, she was discharged home.
During the follow-up of the patient by telephone, at 24 and 48 hours postoperatively, the patient remained asymptomatic, with no recurrence of arrhythmia.
At 6 months of evolution of the patient, he underwent laparoscopic cholecystectomy, under balanced inhalation general anesthesia, without intercurrences, remaining in sinus rhythm.
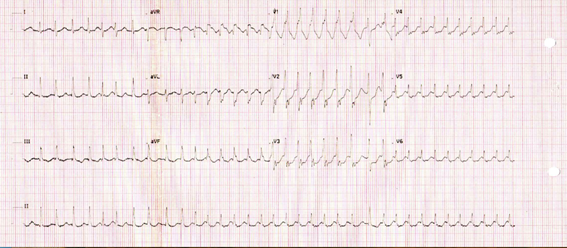
Figure 1: EKG in atrial fibrillation with aberrant AV conduction rate dependent, high ventricular response HR at 220 bpm
DISCUSSION
Ambulatory surgical procedures are increasingly frequent in Peru, although there are very few independent ambulatory surgery centers, this clinical case was presented in one of them. In recent years, due to a marked development of surgeries and new techniques in anesthesia with ultra-short-acting drugs, as well as an optimal perioperative evaluation and preparation of the patient, both for anesthesia and for surgery. The improvements in the recovery unit have contributed to this being possible,1,2however some procedures are complicated and anesthesiologists must be attentive to these medical events, which may occur in the perioperative period. It is very important to understand the mechanisms of AF by cardiologists, anesthesiologists and surgeons, as well as the treatments to provide timely patient care.
The preoperative evaluation, checklist, signed informed consents, preoperative education were completed. The technique used was intravenous at doses according to the monitoring of anesthetic depth, with no intercurrences in the intraoperative period, however 30 'after arriving at the anesthetic recovery unit, he presented tachycardia and later atrial fibrillation.
Postoperative atrial fibrillation (POAF), we wonder what the prevalence is in patients without a history of AF, in outpatient procedures or non-cardiac surgeries. Koren O, et al.3carried out a descriptive study, which included 24,125 patients undergoing non-cardiac surgery and found a prevalence of 2.69 x 1000 patients, more frequent in hip fixation and abdominal surgeries. Bessissow A. et al4report an incidence of 3% in adult patients for non-cardiac surgeries, with electrical cardioversion being the most effective treatment to restore sinus rhythm with a success rate of 69.2%3.
The pathophysiology of AF in non-cardiac surgeries is not well understood, it is believed that in most cases AF is caused by the combination of multiple mechanisms and factors, first the activation of the sympathetic system, due to the stress of surgery and catecholamine release, other clinical circumstances such as hypovolemia, intraoperative hypotension, anemia, trauma and pain, can affect sympathetic activity and cause metabolic imbalances (hypoglycemia or electrolyte disturbances).
Hypoxia can also cause arrhythmia, due to vasoconstriction of the pulmonary vein and increased pressure in the right ventricle. Likewise, hypervolemia could cause an increase in intravascular volume, which causes a stretching of the right atrium.
Likewise, Bessissow A et al.4correlated the presence of arrhythmias with elevated inflammatory markers, such as C-reactive protein (CRP), white blood cells, and interleukins. In this case, apart from surgical stress, none of these factors were present, it was a relatively bloodless surgery, in a young patient without major hemodynamic changes, according to the registry, AF did not present intraoperatively either.
Parida S Et. Al.5, make a review on tachyarrhythmias, explored a temporal relationship between medications in the perioperative period, the mechanisms, as well as the drugs that could trigger them, evaluated the factors and classified them according to the patient, pathology, position, The pharmacology and the procedure, regarding the medications, mentions inhalational anesthetics, atropine, spinal anesthesia and concludes that the choice of anesthetic agents may be important to mitigate the incidence of tachyarrhythmias. However, none of the agents that the authors mention as not recommended were used.
Kounis N et al.6conducted a review where it is mentioned that AF affects 35 million people in the world annually, it is a common postoperative complication that can occur spontaneously during general and local anesthesia.
The authors consider that the higher incidence of AF is correlated with the activation of the autoimmune system, paroxysmal atrial fibrillation (AF) is the most common of arrhythmias, they occur in 3% of patients, many resolve spontaneously but if AF paroxysmal persists, the risk of stroke in one year is 1.5%, compared to 0.3%, of those who do not have it. In addition, heart failure, myocardial infarction, and cardiac arrest can occur in patients with paroxysmal AF.7Therefore, the follow-up of these patients is very important to prevent later complications.
Likewise, in a systematic review,8) whose main objective was to identify the incidence of new-onset AF after general surgery, the secondary objective was to know the risk factors and associated results (mortality and thromboembolic disease), not studied patients with a history of AF. The incidence of postoperative AF was associated with chest and abdominal operations, as well as a duration of more than 600 min. However, they suggest multicenter studies, in order to better stratify risk factors.
We think, what could have triggered this atrial fibrillation, in terms of anesthesia the intravenous technique was used.
There are many studies on the safety of this technique, among them, propofol and remifentanil have very few arrhythmogenic properties, Propofol9does not alter HR, it has a small negative chronotropic effect. Likewise, opioids reduce HR through a central mechanism that decreases sympathetic tone and increases vagal tone.
The European Society of Cardiology,10classifies AF into 5 types: recently diagnosed without previous history, paroxysmal that lasts less than 7 days with or without intervention, persistent that lasts more than 7 days, long-term persistent that lasts more than one continuous year and the permanent one that is accepted by the patient and the doctor and no further attempts will be made to restore or maintain sinus rhythm.
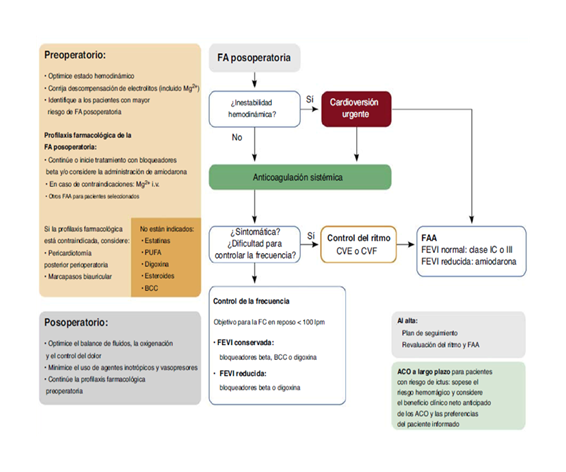
As recommended10(Fig. 3) the acute treatment of FAPO. will depend on the hemodynamic status. If we have signs of instability, such as hypotension, hypoperfusion, sensorial disorder, among others, electrical cardioversion (ECV) will be performed.
If we have signs of hemodynamic stability and symptoms persist or we have difficulty controlling the heart rate, we can choose a rhythm control strategy. This can be achieved by pharmacological cardioversion with group I-C or III antiarrhythmic drugs or ECV. In the case described, an initial attempt was made with amiodarone, in a loading dose followed by intravenous infusion and two hours later, palpitations associated with dyspnea persisted and, as recommended by clinical practice guidelines, ECV was performed effectively.
Cardiovascular events are the third most frequent problem in post-anesthesia care units11.
It is concluded that perioperative AF does not induce any adverse heart disease such as cardiogenic shock.12
The long-term prognosis is variable and the treatment options are diverse, from the simple control of symptoms, to the most aggressive strategies, such as ablation with three-dimensional electroanatomic mapping, which requires the identification of high-risk patients, who they will require a more aggressive treatment, from the beginning of the evaluation of their FA13.
If we speak in terms of primary prevention, we would consider a FAPO high risk, in terms of the association with comorbidities and complications. Therefore, predicting the incidence of postoperative AF would be useful for short- and long-term management, such as anticoagulation therapy.
CONCLUSION
In this case, despite the adequate patient selection, the surgical and anesthetic methods, the picture of POAF was presented, early diagnosis and timely treatment was made, with cardioversion due to hemodynamic instability, the patient was young, without significant medical history. The purpose of this review is to take into account a preventive and therapeutic approach, have a comprehensive vision in the treatment of AF, in outpatient surgery centers and provide our patient’s timely care.
REFERENCES
1. Lee JH . Anesthesia for ambulatory surgery. Korean Journal of Anesthesiology.KoreanSocietyofAnesthesiologists;2017;70(4):398-406.Availablefrom: /pmc/articles/PMC5548941/. DOI: https://doi.org/10.4097/kjae.2017.70.4.398. [ Links ]
2. Okocha O, Gerlach RM, Sweitzer B. Preoperative Evaluation for Ambulatory Anesthesia What, When, and How? Anesthesiology Clincs W.B. Saunders;2019;37(2):195-213.Availablefrom:https://pubmed.ncbi.nlm.nih.gov/31047124/ DOI:https://doi.org/10.1016/j.anclin.2019.01.014. [ Links ]
3. Koren O, Hakim R. Israeli A, et al. Postoperative New-Onset Atrial Fibrillation following Noncardiac Operations: Prevalence, Complication, and Long-Term MACE. CardiologyResearchandPractice2020(10)1-6.ID8156786. . https://doi.org/10.1155/2020/8156786. [ Links ]
4. Bessissow A, Khan J, Devereaux J, et al. Postoperative atrial fibrillation in non-cardiac and cardiac surgery: An overview. Journal of Thrombosis and Haemostasis2015;13(1):304-312.Availablefrom: https://pubmed.ncbi.nlm.nih.gov/26149040/ DOI: 10.1111/jth.12974. [ Links ]
5. Parida S, Thangaswamy Ch, Cardiac tachyarrhythmias and anaesthesia: General principles and focus on atrial fibrillation. Indian Journal of Anaesthesia. Indian Society of Anaesthetists 2017;61:712-20. Available from: /pmc/articles/PMC5613596/. DOI:10.4103/ija.IJA_383_17. [ Links ]
6. 6.Kounis N, Koniari I,Tzanis G, et al, Anaphylaxis-Induced Atrial Fibrillation and Anesthesia: Pathophysiologic and Therapeutic Considerations. Annals ofCardiacAnaesthesia2020;23:1-6. Availablefrom:/pmc/articles/PMC7034217/.DOI:10.4103/aca.ACA_100_19. [ Links ]
7. Sellers D, Srinivas C, Djaiani G. Cardiovascular complications after non-cardiacsurgery.Anaesthesia2018;73(1):34-42.Availablefrom: https://pubmed.ncbi.nlm.nih.gov/29313903/.doi:10.1111/anae.14138 . [ Links ]
8. Chebbout, Heywood EG, Drake TM, Wild JR et alt. A systematic review of the incidence of and risk factors for postoperative atrial fibrillation following general surgery.Anaesthesia2018;73(4):490-498.Availablefrom: https://pubmed.ncbi.nlm.nih.gov/29105078/.doi:10.1111/anae.14118 . [ Links ]
9. Wafae B, Da Silva R, Veloso H. Propofol for sedation for direct current cardioversion. Annals of Cardiac Anaesthesia. 2019 Apr-Jun;22(2):113-121. Availablefrom:https://pubmed.ncbi.nlm.nih.gov/30971591/. doi: 10.4103/aca.ACA_72_18. [ Links ]
10. Hindricks G, Potpara T, Dagres N, Bax JJ, Boriani G, Dan GA, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). EurHeartJ.2021Feb1;42(5):373-498.Availablefrom: https://pubmed.ncbi.nlm.nih.gov/32860505/.Doi:10.1093/eurheartj/ehaa612. [ Links ]
11. Cardiovascular problems in the post-anesthesia care unit (PACU) - UpToDate [Internet]. [cited 2021 May 20]. Available from: https://www.uptodate.com/contents/cardiovascular-problems-in-the-post-anesthesia-care-unit-pacu?search=Cardiovascular problems in the post-anesthesia careunit(PACU).&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. DOI: 10.5327/Z1414-4425201700040007 [ Links ]
12. Higuchi S, Kabeya Y, Matsushita K, Arai N, Tachibana K, et alt. Incidence and complications of perioperative atrial fibrillation after non-cardiac surgery for malignancy. PLoSOne.2019May7;14(5):e0216239.Availablefrom: https://pubmed.ncbi.nlm.nih.gov/31063466/. Doi: 10.1371/journal.pone.0216239. [ Links ]
13. Compagnucci, P., Volpato, G., Falanga, U, Cipolletta L, Conti M, Grifoni G,et al. Recent advances in three-dimensional electroanatomical mapping guidance for the ablation of complex atrial and ventricular arrhythmias. J Interv Card Electrophysiol (2020).Availablefrom:https://pubmed.ncbi.nlm.nih.gov/32451799/https://doi.org/10.1007/s10840-020-00781-3. [ Links ]
Received: June 17, 2021; Accepted: July 24, 2021











 texto em
texto em