Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.1 Lima ene./mar 2022 Epub 31-Dic-2021
http://dx.doi.org/10.25176/rfmh.v22i1.4060
Original article
Effects of two resistance exercise programs on the health-related fitness of obese women with pain symptoms in the knees: An experimental study
1Graduate Program of Health Promotion of Cesumar University, Maringa, Parana, Brazil.
2Interdisciplinary Laboratory of Intervention in Health Promotion, Maringa, Parana, Brazil.
3Assaly Institute of Personalized Medicine
Introduction:
Overweight negatively impacts the cardiovascular system and osteomyoarticular, promoting pain in the joints of the lower limbs. Therefore, strategies have been applied to reduce overweight through lifestyle changes.
Objective:
To investigate the effects of two multidisciplinary intervention programs on the health-related physical fitness of obese women with pain symptoms in the knees.
Methods:
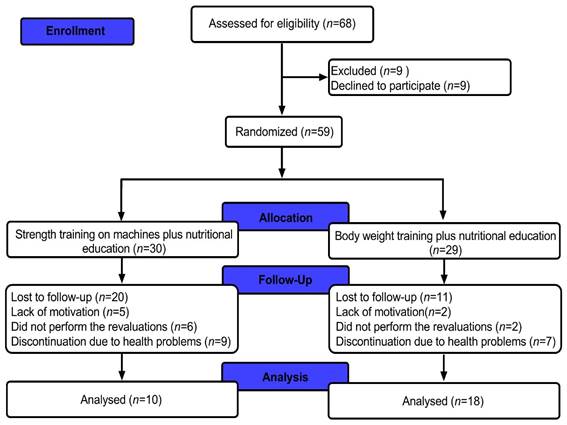
Women between 40 and 59 years of age with obesity (n=59) were evaluated pre- and post-intervention in terms of anthropometry, body composition, physical fitness, level of disability in the knee and hip, and health-related quality of life. A randomized experimental study of parallel groups was conducted for 8 weeks, using two resistance exercise programs and food reeducation. All participants received the same nutritional interventions. For physical exercises, the participants were randomized into two groups: G1, the “strength group” using machines (n=30), and G2, the “body weight” group (n=29). Twenty-eight women (G1, n=18; G2, n=10) were included in the final analyses. This study was approved by Ethics Local Committee. The groups and time were evaluated using two-way analysis of variance with repeated measures. A p<0.05 was assumed for all analyses.
Results:
A time effect was identified, with higher values for maximum isometric lumbar traction strength after the intervention period in both groups (p<0.05). However, no significant differences were identified among the other variables investigated (p>0.05).
Conclusion:
The absence of significant results for all variables, except maximum isometric lumbar traction, may be justified by the moderate adherence of the participants to interventions (approximately 59%-66%) since the study was conducted during the period of social isolation (COVID-19). However, it is believed that the intervention models were positive in maintaining the variables studied.
Keywords: Adiposity; Osteoarthritis; Health promotion (Source : MeSH - NLM).
INTRODUCTION
Obesity unfavorably affects different organ systems, such as cardiovascular and osteomyoarticular1, reducing the ability to work2, increasing public spending3, and increasing the number of morbidity and mortality worldwide from noncommunicable chronic diseases4; therefore, the picture is difficult to reverse. Given this, public policies that work with health promotion in the physical and nutritional spheres (lifestyle changes), with the encouragement of regular and systematized physical activity (PA) and healthy nutrition, are substantial for longevity with health and quality of life.
Knee osteoarthritis is one of the osteomyoarticular dysfunctions related to obesity. This dysfunction is characterized by persistent joint pain and limitation of movement, causing a reduction in functional capacity and quality of life, which often culminates in the indication for knee arthroplasty5. The respective causes, as mentioned earlier, may be related to biomechanical (joint overload) and chemical (inflammatory marker) factors5. For the management of knee osteoarthritis and obesity, studies have pointed out that a multidisciplinary care plan may offer control of disease progression, weight reduction, and, consequently, improvement of health-related components1.
According to the European League Against Rheumatism (EULAR), nutritional education and physical training are recommended for managing obesity and osteoarthritis to decrease body weight (BW) and improve clinical conditions such as pain, functional disability, stiffness, and joint mobility6. Recent scientific evidence shows that resistance training models, using apparatus in the weight room and training with the body’s resistance (commonly referred to as "body weight training"), improve health-related fitness in people with obesity7,8. However, there is no consensus in the literature about which method or model of resistance training may be more effective in reducing algae and improving health-related fitness and quality of life in overweight or obese women.
Thus, considering that “BW” training is a cost-effective model since it uses only BW and accessories9, it is conjectured that this method may be incorporated into the routine for the recovery of health conditions and reduction of disability in overweight or obese people. Finally, it was observed that BW improved health-related physical fitness and reduced pain. In that case, cost-effective strategies can be incorporated on a large scale to improve the quality of life of this population, considering a model of low infrastructural investment.
Therefore, this study aimed to investigate the effects of two multidisciplinary intervention programs, distinguishing between the types of resistance training performed, that is, resistance training on machines or resistance training with BW. It is believed that both intervention models can improve health-related physical fitness and quality of life for obese women with knee pain symptoms.
METHODOLOGY
Experimental design
This is an experimental, longitudinal, randomized, parallel group, and repeated-measures study. The research was approved by the Local Ethics Committee at UniCesumar University, in southern of Brazil, according to the following opinion: 30976420.4.0000.5539. The project was advertised via printed media, the Internet, and television, inviting women between 40 and 59 years of age, within the inclusion criteria, to participate in the research project.
The inclusion criteria were as follows: (i) participants with body mass index (BMI) ≥ 30.00-34.9 kg/m²; (ii) female sex, aged 40-59 years; (iii) presenting three or more of the criteria, namely, morning stiffness lasting < 30 min, crepitus, bone lesion, and no palpable knee lesion, according to the EULAR; (iv) availability to participate in the interventions, three times a week, for 8 weeks; (v) be able to practice PA, via medical clearance; (vi) not participating in another project focused on weight loss; (vii) not performing any nutritional diet; and (viii) agreed and signed the informed consent form (ICF).
The exclusion criteria included the following: (i) participants who underwent knee arthroplasty in the affected joint or any other surgical procedure in the lower limbs in the last 6 months; (ii) who presented with rheumatologic conditions; (iii) who underwent medicated infiltrations in the knee in less than 3 months; (iv) who presented with thrombotic episodes; (v) with decompensated heart disease; (vi) using a pacemaker or similar device; (vii) with uncontrolled hypertension; (viii) with a confirmed diagnosis of cancer; (ix) with dermatological lesions; (x) unable to walk or use a walking aid; and (xi) unable to understand and complete the proposed instructions and evaluations.
Women who met the inclusion criteria were selected and instructed about the research procedures, signed the ICF, and were subsequently randomized (www.randomizer.org) into two experimental groups: strength training on machines or BW training. The sample calculation indicated that 10 people per group would be sufficient to present an α = 0.05 and β = 80%, whose variables were BMI and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). A flowchart of the present study is presented inFigure 1.
Systematization of assessments and interventions
The participants were evaluated pre- and post-intervention in three stages: (i) medical consultation, with general physical examination and interview with a physician; (ii) after 48 h, the performance of anthropometry and body composition; and (iii) application of physical tests and completion of health-related questionnaires. The evaluation process is presented in the following, according to the order of the days mentioned earlier. The interventions were performed three times a week, lasting 60 min (plus nutritional counseling once a week for 30 min), over 8 weeks of a multi-professional project involving nutrition, physical education, and physical therapy professionals.
Anthropometry and body composition
Body composition was measured using an InBody 570® bioimpedance device (InBody®, Body Composition Analyzers, South Korea) to evaluate the following parameters: (i) BW (kg), (ii) BMI, (iii) body fat mass (FM), (iv) body fat percentage (BFP), and (v) skeletal muscle mass (SMM). Height was measured using a Sanny stadiometer (Standard®) following Heyward’s standardization10. The participants followed the protocol published by Branco et al.11to perform the measurements.
Health-related fitness tests
Health-related fitness tests were performed in the following order: (i) maximum isometric handgrip strength (MIHS), (ii) maximum isometric lumbar traction strength (MILTS), (iii) flexibility on the Wells bench, (iv) elbow flexion and extension, (v) abdominal strength endurance, and (vi) aerobic capacity.
To evaluate MIHS, a Takei Physical Fitness Test® (Tokyo, Japan) TKK 5101 dynamometer was used, following the standardization proposed by Branco et al.12.
To perform the MILTS, a Takei Physical Fitness Test® (Tokyo, Japan) model TKK 5002 dynamometer was used, following the protocol used by Branco et al.12.
The Wells bench test was performed following the protocol published by Wells and Dillon13.
According to the Marinho and Marins protocol, we used the elbow flexion and extension test to measure muscle strength and endurance14. The 60-s abdominal test was also performed according to Ribeiro et al.15.
The 6-min walk test was performed according to the American Thoracic Society standardization16. The test was performed at least 2 h after meals, and the participants were instructed to wear comfortable clothes and shoes, in addition to keeping their usual medication. Before the test, the participants took a rest period of at least 10 min. With the data collected from the test, peak oxygen consumption (VO2peak) was calculated according to the following equation: VO2peak (mL.kg-1.min-1) = (0.02 distance [m]) - (0.191 x age [years]) . (0.07 body weight [kg]) . (0.09 height [cm]) + (0.26 x SD [x 10-3]) + 2.45, where m is the distance in meters, year is the number of years, kg is kilogram, cm is centimeters, and SD is the double product, which is the systolic blood pressure multiplied by the heart rate17. All physical tests were interspersed with rest periods so that one physical response did not negatively impact the other subsequent responses.
Application of the questionnaires
The following questionnaires were used: the Medical Outcomes Study 12 (SF-12) short version validated for Brazilians18; WOMAC, validated for the Brazilian population19; and International PA Questionnaire (IPAQ) in a short version, adapted and applied as an interview20.
Multiprofessional interventions
Nutritional interventions: After the initial process, guidance on healthy eating habits was offered through educational lectures and encouragement to participate in the two practices once a week. The nutritional interventions were focused on instructing the participants regarding nutritional aspects: (i) food pyramid; (ii) nutrient density of foods; (iii) nutritional composition of foods; (iv) association of food with health and quality of life; (v) differences between diet and light foods; and (vi) differences between fresh, minimally processed, processed, and ultra-processed foods. Additionally, the participants were instructed to fill out the food record of 3 nonconsecutive days, one day on the weekend and before and after 8 weeks of intervention. Subsequently, the food record responses were calculated using Avanutri® software (version 2004, Avanutri Equipamentos de Avaliação Ltda., Três Rios, Rio de Janeiro, Brazil).
Physical exercises: Resistance exercises were performed three times a week, alternating in sessions A and B. The exercise protocol followed the American College of Sports Medicine21, with appropriate volume and intensity of effort for obese women with no previous experience in resistance exercise.
Table 1shows the exercises performed in trainings A and B for the BW group. Table 2presents the prescription of the resisted exercises in training series A and B for the strength training on machines group.
Table 1. Prescription of the “body weight” exercises performed during 8 weeks of intervention
| Training program A prescription | Training program B prescription | ||||
| Exercises | Series | Repetitions | Exercise | Series | Repetitions |
| 1) General warm-up (low skipping, high skipping, side runs, front, and back runs) | 5 min | * | 1) General warm-up (low skipping, high skipping, side runs, front, and back runs) | 5 min | * |
| 2) Half Squat | 3 | 12 | 2) Rowing in TRX (neutral grip) | 3 | 12 |
| 3) Up and down on the tire or step | 3 | 12 | 3) Pull rope (tied to the tire) | 3 | 12 |
| 4Stiffwith dumbbells | 3 | 12 | 4) Push-ups (knee on floor) | 3 | 12 |
| 5) Half squat with Swiss ball between thighs (squeeze in isometrics) | 3 | 12 | 5) Half squat with medicine ball tosses upwards (catch and toss) | 3 | 12 |
| 6) With elastic band squatting laterally Performing a leg abduction | 3 | 12 | 6) Lumberjack movement (with ball) | 3 | 12 |
| 7) Standing hip | 3 | 12 | 7) Biceps curl with wall-ball | 3 | 12 |
| 8) Calf raises | 8) Triceps on bench | ||||
| 9) Low-intensity aerobics (jogging and then walking) | 10 min | * | 9) Straight abdomen on the ground | 3 | 12 |
Table 2. Prescription of "strength training on machines" exercises performed during 8 weeks of intervention.
| Training program A prescription | Training program B prescription | ||||
| Exercises | Series | Repetitions | Exercise | Series | Repetitions |
| 1) General warm-up | 5 min | Treadmill or bicycle | 1) General warm-up | 5 min | Treadmill or bicycle |
| 2) Hack squat | 3 | 12 | 2) Front Handle | 3 | 12 |
| 3) Leg extension | 3 | 12 | 3) Low Row | 3 | 12 |
| 4) Leg curl machine | 3 | 12 | 4)Chest-press | 3 | 12 |
| 5) Adduction machine | 3 | 12 | 5) Front flyer | 3 | 12 |
| 6) Abduction machine | 3 | 12 | 6) Shoulder press machine | 3 | 12 |
| 7) Calf raises | 3 | 12 | 7) Bicep’s curl | 3 | 12 |
| 8) Standing hip | 8) Tricepspulley | 3 | 12 | ||
| 9) Low intensity aerobics | 10 min | Treadmill or bicycle | 9) Straight abdomen on the ground | 3 | 12 |
Monitoring of physical training sessions: The rating of perceived exertion (RPE) was measured 30 min after each intervention session, following the recommendations proposed by Foster et al.22. The internal training load (ITL) was calculated by multiplying the RPE and time in minutes. The rating of perceived recovery (RPR) was measured before each exercise session23. All participants were familiarized with the psychometric scales before and during the study.
Statistical analysis
Data are presented as means, standard deviations, and 95% confidence intervals (CIs). Levene’s test was used to identify the homogeneity of the data, and the Shapiro-Wilk test was used to test for normality. Once data homogeneity and normality were confirmed, a two-way (group × time point) analysis of variance was performed using the Bonferroni test if necessary. Sphericity was tested using Mauchly’s test, and the Greenhouse-Geisser correction was used if necessary. For all analyses, the established significance level was set to 5%. Statistica, version 12.0 (StatSoft, USA), was used for all statistical analyses.
RESULTS
This study verified the participation in the interventions of 59.0 ± 27.7% for the strength training on machines group and 66.2 ± 27.9% for the BW training group, over 8 weeks of intervention. The mean ages were 45.1 ± 5.0 and 45.7 ± 49.9 years for the strength training on machines group and the BW training group, respectively, with no significant difference between them (p>0.05). Moreover, 64% had higher education among the participants, 32% had completed high school, and 4% had incomplete elementary school education. The family income averages were 40% up to 3 minimum wages and 28%, 16%, 8%, and 4% up to 3, 9, 12, and 15 minimum wages, respectively. For all variables investigated, no significant differences were observed in the baseline values (p>0.05). no significant difference was detected among RPE, ITL, and RPR responses at the same points of comparison, suggesting that training intensity and recovery were similar between the groups (p>0.05). In addition, no significant difference was observed to food record data (p>0.05).Table 3presents the anthropometric and body composition responses of the participants in this study.
Table 3. Anthropometry and body composition performed by the participants of the present study.
| Strength training on machines | Body weight training | |||||||
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | |||||
| Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | |
| Body Weight (kg) | 89.9 ± 20.6 | 80.5-99.1 | 90.0 ± 20.4 | 80.8-99.1 | 87.1 ± 19.4 | 39.2-49.0 | 86.8 ± 18.9 | 98.6-75.1 |
| Height (cm) | 163.3 ± 7.7 | 159.8-166.8 | 163.3 ± 7.7 | 159.8-166.8 | 164.1 ± 10.5 | 157.6-170.6 | 164.1 ± 10.5 | 157.6-170.6 |
| BMI (kg/m²) | 33.6 ± 6.8 | 30.5-36.6 | 34.0 ± 6.5 | 31.0-36.9 | 32.3 ± 6.7 | 28.1-36.4 | 32.1 ± 6.7 | 27.9-36.2 |
| SMM (kg) | 27.4 ± 4.8 | 25.2-29.6 | 27.4 ± 4.9 | 25.2-29.6 | 27.9 ± 3.8 | 25.5-30.2 | 28 ± 3.8 | 25.7-30.4 |
| FM (kg) | 41.3 ± 15.2 | 34.5-48.1 | 40.9 ± 15.3 | 34.5-48.1 | 36.7 ± 14.6 | 27.7-45.7 | 36.2 ± 14.3 | 27.3-45.0 |
| BFP (%) | 44.3 ± 7.9 | 40.8-47.9 | 45.4 ± 10.9 | 40.5-50.3 | 41.2 ± 6.7 | 37.0-45.3 | 40.1 ± 7.0 | 35.8-44.5 |
Note: data are expressed by mean and (±) standard deviation (SD); CI = 95% confidence interval; BMI = body mass index; SMM = skeletal muscle mass; FM = fat mass; BFP = body fat percentage;p>0.05 for all comparisons.
For MIHS-R, MIHS-L, flexibility, abdominal test, elbow flexion and extension, and VO2peak, no significant differences were observed after 8 weeks of intervention (p>0.05). However, there was a time effect, with a significant increase in MILTS after the intervention (p<0.05), as shown inTable 4
Table 4. Physical tests performed by the participants of the present study from both intervention groups.
| Strength training on machines | Body weight training | ||||||||
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | ||||||
| Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | ||
| MIHS-R (kgf) | 30.8 ± 7.1 | 27.6-34.0 | 29.2 ± 8.0 | 25.5-32.8 | 33.2 ± 5.4 | 29.9-36.5 | 33.2 ± 5.3 | 29.9-36.5 | |
| MIHS-L (kgf) | 28.7 ± 5.7 | 26.1-31.3 | 30.4 ± 5.9 | 27.7-33.0 | 32.5 ± 4.8 | 29.4-35.5 | 31.7 ± 4.8 | 29.4-35.5 | |
| MILTS (kgf)* | 72.6 ± 20.5 | 63.4-81.8 | 81.3 ± 23.1 | 70.9-91.7 | 79.5 ± 26.1 | 95.7-63.3 | 81.0 ± 25.2 | 65.4-96.6 | |
| Flexibility (cm) | 25.2 ± 7.0 | 22.1-28.4 | 26.8 ± 8.2 | 23.1-30.4 | 26.8 ± 7.5 | 22.2-31.4 | 27.5 ± 6.5 | 23.4-31.5 | |
| Abdominals (reps) | 20.9 ± 9.9 | 16.5-25.4 | 23.6 ± 9.2 | 19.5-27.8 | 23.1 ± 7.5 | 18.4-27.8 | 25.2 ± 11.7 | 17.9-32.5 | |
| Push-ups (reps) | 23.2 ± 7.3 | 19.9-26.5 | 23.8 ± 7.4 | 20.5-27.1 | 25.7 ± 4.0 | 23.2-28.2 | 26.4 ± 4.1 | 23.9-28.9 | |
| VO2peak (mL/kg/min) | 18.1 ± 3.0 | 16.8-19.5 | 17.7 ± .4.0 | 16.2-19.2 | 18.2 ± 2.7 | 16.5-19.9 | 15.1 ± 5.4 | 11.8-18.5 | |
Note: data are expressed by mean and (±) standard deviation (SD); CI = 95% confidence interval; MIHS-R = maximum isometric handgrip strength of right rand; MIHS-L = maximum isometric handgrip strength of left hand; MILTS = maximum isometric lumbar-traction strength; * = time effect with higher values in the post-intervention period, p < 0.05.
No significant differences were observed in pain, joint stiffness, and physical ability after completing the WOMAC questionnaire among the study participants (p>0.05).Table 5shows the responses to the SF-12 questionnaire for the two experimental groups. No significant differences were observed in the SF-12 questionnaire for physical and mental health domains over 8 weeks of intervention (p>0.05). The same occurred when filling out the IPAQ questionnaire; that is, no significant differences were observed in the level of PA during 8 weeks of intervention (p>0.05). The only difference was the increase in the PA level on the days of intervention, that is, on Mondays, Wednesdays, and Fridays, which was already expected since the participants performed resistance exercises on these days.
Table 5. WOMAC (Western Ontario and McMaster Universities) and SF-12 (Medical Outcomes Study) scores of the participants the participants of the present study from both intervention groups.
| Strength training on machines | Body weight training | ||||||||
| WOMAC Questionnaire | |||||||||
| Domains | Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | |||||
| Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | ||
| Pain (0-20) | 4.0 ± 2.8 | 2.6-5.4 | 2.2 ± 3.8 | 0.4-4.0 | 3.6 ± 4.1 | 1.0-6.2 | 3.8 ± 2.9 | 2.0-5.6 | |
| Joint Stiffness (0-8) | 1.4 ± 1.4 | 0.8-2.1 | 1.1 ± 1.5 | 0.4-1.8 | 1.6 ± 1.9 | 0.4-2.8 | 1.7 ± 1.4 | 0.8-2.6 | |
| Physical Capacity (0-68) | 10.6 ± 11.0 | 5.4-15.9 | 6.5 ± 10.1 | 1.7-11.3 | 14.9 ± 18.2 | 3.7-26.1 | 8.5 ± 7.5 | 3.8-13.2 | |
| SF12 Questionnaire | |||||||||
| Domains | Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | |||||
| Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | Mean (±) SD | CI 95% | ||
| Physical Health | 25.1 ± 3.2 | 23.6-26.6 | 26.1 ± 4.1 | 24.1-28.1 | 25.6 ± 3.0 | 23.7-27.5 | 22.0 ± 4.5 | 19.2-24.8 | |
| Mental Health | 13.6 ± 1.1 | 13.0-14.1 | 13.1 ± 1.2 | 12.5-13.7 | 13.7 ± 1.3 | 12.9-14.5 | 13.6 ± 1.1 | 12.9-14.3 | |
Note: data are expressed by mean and (±) standard deviation (SD); CI = 95% confidence interval; p>0.05 for all comparisons.
DISCUSSION
The present study aimed to analyze the different anthropometric variables and body composition in physical fitness in obese women with knee pain symptoms who underwent two modalities of resistance exercises. In this sense, the following responses were observed: (i) absence of significant differences in the variables of BW, height, BMI, SMM, FM, and BFP for both experimental groups; (ii) absence of significant differences in the tests of physical fitness for both experimental groups (MIHS-R, MIHS-L, abdominals in 60 s, elbow flexion and extension, and VO2peak); (iii) the only difference observed for the health-related fitness tests was for the MILTS, with significant improvement for both experimental groups; (iv) no differences in the responses of the WOMAC, SF-12, and IPAQ questionnaires; (v) no differences in the responses of the food record; and (vi) no differences in the responses of the RPE, ITL, and RPE between the two resistance training models.
The absence of differences in the anthropometric and body composition variables can be explained by the low energy expenditure promoted by the training sessions and moderate adherence to the interventional process. Energy expenditure is dependent on the following factors: thermal effect of food, resting metabolic rate (RMR), and PA level; the latter is dependent on the energy expenditure of structured and unstructured physical activities during the day24.
However, weight loss is not linear since the body tends to self-regulate, even with adequate nutrition and regular PA practice, depending on physiological factors25. According to MacKenzie-Shalders et al.26, resistance training does not accelerate the metabolism to the point of obtaining high weight loss because a gain of 1 kg of muscle increases the caloric expenditure by 13 kcal, a factor that alone does not promote weight loss; therefore, the weight loss process is complex and multifactorial and involves lifestyle changes. Weight loss must constantly be associated with reduced caloric intake and increased levels of PA (structured and unstructured activities throughout the day). Therefore, in this situation, the literature points out that the reduction in body fat is still small in interventions of only 8 weeks’ duration27. An aggravating factor for the absence of changes in the anthropometric and body composition variables can be justified by the moderate compliance of participants during the 8-week intervention (approximately 59%-66%). On the other hand, when considering that the interventions were performed in the most restricted period of the pandemic in the locality where the project was conducted, it is believed that the results were satisfactory since there was no adverse modification of the anthropometric and body composition variables, since, during the pandemic, an increase in BW was observed2. Although no significant differences were observed for the anthropometric and body composition variables in this study, Swift et al.28emphasized that a physical training program for treating obesity is essential for maintaining muscle mass in the long term.
It is essential to highlight that activities in home-office mode (to contain the pandemic) probably presented low energy expenditure, and consequently, the body in the medium and long term, with reduced energy expenditure and increased caloric intake, provided more significant accumulation of body fat. Although no differences were observed in the main variables investigated in this study, physical, nutritional, and behavioral changes are linked to long-term work; if maintained, the intention to change behavior will probably improve practitioners’ health and quality of life6. As a result, a reduction in sedentary time is pertinent, reducing sitting time with daily life activities at home and at work with slight changes, that is, choosing to use the stairs rather than the elevator, standing up every 30 or 60 min and then walking or stretching, walking further instead of using the car or public transport, and using the daily step counter and setting goals, in addition to reducing the salt, sugar, and fat intake. Therefore, tangible goals can be arranged to change a healthy lifestyle.
Another relevant point is the age factor: it is known that the aging process is natural, resulting in physiological changes, reduced physical and motor capacities, degenerative processes, increased body fat, and reduced muscle mass. Therefore, the components of physical fitness need to be stimulated to slow these reductions and improve physical and mental health8. Thus, although the participants missed an average of 35%-40% of the interventions, the MILTS increased significantly. The increase in the MILTS is a highly positive response since back pain considerably affects the Brazilian and global populations29.
It is also worth mentioning that the reduction in muscle mass, fat accumulation, and poor posture cause lower back pain and pain in some joints, which, in turn, can modify the physiological curvature, leading to weakness and pain in the postural muscles, in addition to a muscular imbalance of the trunk and lower limbs29. In obese individuals, reduced strength and increased fatigue are evident when exposed to complex tasks that require high intensity30. In the present study, the significant improvement in the MILTS contributed to the muscles responsible for posture, reducing the risks of future muscle pain and fatigue. Moreover, some studies have shown that an active lifestyle is beneficial because participants develop a delay in the onset of functional, cardiorespiratory, postural, balance, and muscle endurance limitations to perform daily tasks with greater competence, preventing falls and fractures31. For Kocjan and Sarabon29, the isometric strength of the trunk acts in the maintenance of strength in the core and stabilization and minimizes the overload of the spine, thus generating dynamic postural control and improving the hip angle; however, the pandemic and the changes from work to home-office form, exceeding the hours sitting in the same position, resulted in an increase in back pain complaints. This possibility is supported by Salve and Bankoff31, who state that hours in the sitting position reduce musculoskeletal fitness and increase nonspecific low back pain; therefore, people expend less energy and maintain poor posture. In this sense, the response of the study may be relevant for the reduction of work leaves due to increased pain, restricted movement, and especially muscle fiber atrophy32.
Other studies with comparative approaches between resistance training methods equalized by the main muscle groups, volume, and intensity of training sessions did not find significant differences between the types of intervention33-35. In this sense, Branco et al.34compared the effects of two resistance training methods (conventional weight training vs. BW and accessory training) on body composition, physical fitness, and biochemical measures. Given this, the previous study results showed similar improvements of health-related fitness components, with no significant difference observed between the intervention groups in the condition where training was equalized. To compare different training exercise methods, the equalization of intensity, volume, and primary muscle groups should be considered. In addition, despite the limitations of the psychometric scales, previous studies have reported consistent responses using these resources33-35.
Thus, physical therapists or physical education professionals need to consider motor actions when the training is designed. If many people are being served simultaneously, we suggest using cost-effective resources to serve more people, with less expenditure on equipment and/or accessories. Finally, the three studies cited33-35equalized the main health variables of interest in interventions to combat obesity. In summary, no significant differences were observed between BW and weight training on machines, order of exercises, aerobic or resistance training, and sports practice versus functional training. Although the three studies mentioned earlier presented adolescents as the sample, it is believed that the main factor for comparison and obtaining similar answers refers to the equalization process.
There were no differences in the answers to the WOMAC and SF-12 questionnaires during the intervention period. According to Hurley et al.36, the participants had some beliefs and/or resistance regarding improving pain and physical function, support, adequate assistance, and confidence in performing the exercises. It is noted that the absence of differences in the responses to the SF-12 questionnaire may be associated with the period of social isolation, which may have affected the mental health of the participants (increased anxiety and insecurity and lowered self-esteem)37. Thus, based on the results of this study, it is highlighted that the absence of significant differences cannot be analyzed only by statistical analysis to confirm or reject the eventual benefits of the program for the recovery of the participants’ health conditions. Considering that the process of behavioral changes for adherence to PA practice and the change in the eating pattern is a lifelong process, the first step was performed, referring to the encouragement of PA for groups in physical, nutritional, and psychosocial vulnerability.
CONCLUSION
No significant differences were observed for the anthropometric, body composition, physical fitness variables (except for MILTS), WOMAC, SF-12, IPAQ questionnaires, food record or women’s RPR, ILT, and RPE. The absence of significant differences may be justified by the moderate adherence of the participants to the study since the study was conducted during a period of more restricted social isolation. However, it is believed that the intervention models were positive in any decrease in health components analyzed in the present study.
Acknowledgments:
REFERENCES
1. Andolfi C, Fisichella PM. Epidemiology of Obesity and Associated Comorbidities. J Laparoendosc Adv Surg Tech. 2018; 28(8):919-924. [ Links ]
2. Mehta RK, Cavuoto LA. Relationship between BMI and Fatigability Is Task Dependent. Hum Factors. 2017; 59(5):722-733. [ Links ]
3. Van Nuys K, Globe D, Ng-Mak D, Cheung H, Sullivan J, Goldman D. The Association between Employee Obesity and Employer Costs: Evidence from a Panel of U.S. Employers. Am J Heal Promot. 2014; 28(5):277-85. [ Links ]
4. Ministério da Saúde. Vigitel Brasil 2019. Vigitel Brasil 2019 : vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico : estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados.2020. [ Links ]
5. Bennell KL, Nelligan RK, Kimp AJ, Wrigley T V., Metcalf B, Kasza J, et al. Comparison of weight bearing functional exercise and non-weight bearing quadriceps strengthening exercise on pain and function for people with knee osteoarthritis and obesity: Protocol for the TARGET randomised controlled trial. BMC Musculoskelet Disord. 2019; 18;20(1):291. [ Links ]
6. Geenen R, Overman CL, Christensen R, Åsenlöf P, Capela S, Huisinga KL, et al. EULAR recommendations for the health professional's approach to pain management in inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018; 77(6):797-807. [ Links ]
7. De Vreede PL, Samson MM, Van Meeteren NLU, Duursma SA, Verhaar HJJ. Functional-task exercise versus resistance strength exercise to improve daily function in older women: A randomized, controlled trial. J Am Geriatr Soc. 2005; 53(1):2-10. [ Links ]
8. Bolognese MA, Franco CB, Ferrari A, Bennemann RM, Lopes SMA, Bertolini SMMG, et al. Group Nutrition Counseling or Individualized Prescription for Women With Obesity? A Clinical Trial. Front Public Heal. 2020; 30;8:127. [ Links ]
9. Silva-Grigoletto ME Da, Resende-Neto AG de, Teixeira CVLS. Treinamento funcional: uma atualização conceitual. Rev Bras Cineantropometria Desempenho Hum. 2020; 22:72646. [ Links ]
10. Heyward VH. Avaliação física e prescrição de exercício: técnicas avançadas. ArtMed. 2013. [ Links ]
11. Branco BHM, Bernuci MP, Marques DC, Carvalho IZ, Barrero CAL, Oliveira FM de, et al. Proposal of a normative table for body fat percentages of Brazilian young adults through bioimpedanciometry. J Exerc Rehabil. 2018; 14(6):974-9. [ Links ]
12. Branco BHM, Andreato LV, Ribeiro ED, de Oliveira HG, Almeida FN, Junior NN. Development of tables for classifying judo athletes according to maximal isometric strength and muscular power, and comparisons between athletes at different competitive levels. Sport Sci Health. 2018; 14, 607-614. [ Links ]
13. Wells KF, Dillon EK. The Sit and Reach - A Test of Back and Leg Flexibility. Res Quarterly Am Assoc Heal Phys Educ Recreat. 1952; 26;23(1):115-8. [ Links ]
14. Marinho BF, Marins JCB. Teste de força/resistência de membros superiores: análise metodológica e dados normativos. Fisioter em Mov. 2012; 25(1):219-30. [ Links ]
15. Ribeiro AH, Fernandes Filho J, Novaes J. A eficácia de três exercícios abdominais para teste de resistência muscular localizada. Fit Perform J. 2002; 1,(1) :37-43 [ Links ]
16. ATS Statement. Am J Respir Crit Care Med. 2002; 166(1):111-7. [ Links ]
17. Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The Six-Minute Walk Test Predicts Peak Oxygen Uptake and Survival in Patients With Advanced Heart Failure. Chest. 1996; 110(2):325-32. [ Links ]
18. Damásio BF, Andrade TF, Koller SH. Psychometric Properties of the Brazilian 12-Item Short-Form Health Survey Version 2 (SF-12v2). Paid 2015; 25(60):29-37. [ Links ]
19. Ferreira C de SB, Dibai-Filho AV, Almeida DO da S, Bassi-Dibai D, Barreto FS, Oliveira AR de, et al. Structural validity of the Brazilian version of the Western Ontario and McMaster Universities Osteoarthritis Index among patients with knee osteoarthritis. Sao Paulo Med J. 2020; 138(5):400-6. [ Links ]
20. Matsudo S, Araújo T, Matsudo V, Andrade D, Andrade E, Oliveira LC, et al. MATSUDO, Sandra et al. Questinário internacional de atividade física (IPAQ): estudo de validade e reprodutibilidade no Brasil. Rev Bras Atividade Física Saúde. 2001; 6(2):5-18. [ Links ]
21. American College of Sports Medicine. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009; 41(3):687-708. [ Links ]
22. Foster C, Florhaug JA, Franklin J, Gottschall L, Hrovatin LA, Parker S, et al. A New Approach to Monitoring Exercise Training. J Strength Cond Res. 2001; 15(1):109-15. [ Links ]
23. Laurent CM, Green JM, Bishop PA, Sjökvist J, Schumacker RE, Richardson MT, et al. A Practical Approach to Monitoring Recovery: Development of a Perceived Recovery Status Scale. J Strength Cond Res . 2011; 25(3):620-8. [ Links ]
24. De Melo CM, Tirapegui J, Ribeiro SML. Human energetic expenditure: Concepts, assessment methods and relationship to obesity. Arq Bras Endocrinol Metabol. 2008; 52(3):452-64. [ Links ]
25. Pontzer H, Raichlen DA, Wood BM, Mabulla AZP, Racette SB, Marlowe FW. Hunter-Gatherer Energetics and Human Obesity. Chehab FF, editor. PLoS One. 2012; 25;7(7):e 40503. [ Links ]
26. MacKenzie-Shalders K, Kelly JT, So D, Coffey VG, Byrne NM. The effect of exercise interventions on resting metabolic rate: A systematic review and meta-analysis. J Sports Sci. 2020; 38(14):1635-1649. [ Links ]
27. Bartholdy C, Christensen R, Kristensen LE, Gudbergsen H, Bliddal H, Overgaard A, et al. Association Between Weight Loss and Spontaneous Changes in Physical Inactivity in Overweight/Obese Individuals With Knee Osteoarthritis: An Eight-Week Prospective Cohort Study. Arthritis Care Res. 2020; 72(3):397-404. [ Links ]
28. Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role of exercise and physical activity in weight loss and maintenance. Prog Cardiovasc Dis. 2014; 56(4), 441-447. [ Links ]
29. Kocjan A, Sarabon N. Assessment of isometric trunk strength - The relevance of body position and relationship between planes of movement. J Sport Sci Med. 2014; 2014;13(2):365-370. [ Links ]
30. Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: A mixed methods review. Cochrane Database of Systematic Reviews. 2018; 7;4(4):CD010842. [ Links ]
31. Salve MGC, Bankoff ADP. Postura corporal: um problema que aflige os trabalhadores. Rev Bras Saúde Ocup. 2003; 28(105-106):91-103. [ Links ]
32. Zacaron K, Dias J, Abreu N, Dias R. Nível de atividade física, dor e edema e suas relações com a disfunção muscular do joelho de idosos com osteoartrite. Rev Bras Fisioter. 2006; 10(3):279-84. [ Links ]
33. Branco BHM, Valladares D, de Oliveira FM, Carvalho IZ, Marques DC, Coelho AA, et al. Effects of the Order of Physical Exercises on Body Composition, Physical Fitness, and Cardiometabolic Risk in Adolescents Participating in an Interdisciplinary Program Focusing on the Treatment of Obesity. Front Physiol. 2019; 6;10:1013. [ Links ]
34. Branco BHM, Carvalho IZ, De Oliveira HG, Fanhani AP, Dos Santos MCM, De Oliveira LP, et al. Effects of 2 Types of Resistance Training Models on Obese Adolescents' Body Composition, Cardiometabolic Risk, and Physical Fitness. J strength Cond Res. 2020; 34(9):2672-2682. [ Links ]
35. Branco BHM, Mariano IR, de Oliveira LP, Bertolini SMMG, de Oliveira FM, Araújo CGA, et al. Sports and Functional Training Improve a Subset of Obesity-Related Health Parameters in Adolescents: A Randomized Controlled Trial. Front Psychol. 2021 21 (11) 589554. [ Links ]
36. Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Ver. 2018. 17;4(4):CD010842. [ Links ]
37. Schmidt B, Crepaldi MA, Dill S, Bolze A, Neiva-silva L, Demenech LM. Impacts on Mental Health and Psychological Interventions related to the New Coronavirus Pandemic (COVID-19). Rev Estud Psicol. 2020. 37: e200063. [ Links ]
Received: August 16, 2021; Accepted: December 07, 2021











 texto en
texto en