Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.1 Lima ene./mar 2022 Epub 31-Dic-2021
http://dx.doi.org/10.25176/rfmh.v22i1.3759
Original article
The lifestyle associated with the control of arterial hypertension and diabetes mellitus in a care center in lima, during the Covid-19 pandemic
1Facultad de Medicina Humana, Universidad Ricardo Palma.
2Instituto de Investigación en Ciencias Biomédicas, Universidad Ricardo Palma.
Introduction:
Hypertension and diabetes mellitus 2 are prevalent diseases. The COVID-19 pandemic has shown the importance of lifestyle in the control of chronic diseases, which can trigger serious complications.
Objectives:
To determine the association between lifestyle and the control of chronic non-communicable diseases: arterial hypertension and diabetes mellitus 2 during the COVID-19 pandemic in patients of an Urgent Care Center.
Methods:
Observational, cross-sectional, and analytical study. A sample of 158 patients, between 30 and 79 years old, was included. Control files and medical records were analyzed, anthropometric values were measured, and lifestyle was assessed using validated scales.
Results:
51.3% were male, an average of 61 years, 57.6% with married marital status, and 51.9% with higher educational level. In the multivariate analysis of patients with arterial hypertension, a significant association between an unhealthy lifestyle and non-control of hypertensive disease was evidenced (PR = 2.538; p = 0.000; 95% CI = 1.608-4.006). On the other hand, the diabetic population obtained a significant association between an unhealthy lifestyle and the lack of control of type 2 diabetes mellitus (PR = 5.498; p = 0.013; 95% CI = 1.440-20.995), in addition to the prevalence of glycemic lack of control in patients with abnormal abdominal girth it was 1.6 times more than in people with normal abdominal girth (PR = 2.623; p = 0.038; 95% CI = 1.057-6.508).
Conclusions:
Lifestyle is significantly associated with the control of arterial hypertension and diabetes mellitus. There is a significant association between abdominal circumference and control of type 2 diabetes mellitus.
Keywords: Lifestyle; hypertension; diabetes mellitus; COVID-19; pandemic; glycemic control; blood pressure. (Source: MeSH NLM).
INTRODUCTION
Chronic non-communicable diseases (NCDs) are part of the leading cause of death worldwide, responsible for at least 41 million deaths. And while they can affect all age groups, an estimated 15 million deaths occur between 30 and 69 years of age. According to figures from the World Health Organization (WHO), cardiovascular diseases cause 17.9 million deaths per year; 9 million for cancer; 3.9 million for respiratory diseases and 1.6 million for diabetes.1
At the national level, arterial hypertension (HT) and diabetes mellitus (DM) are health research priorities because they are part of the health problems that most affect the population and require effective and efficient responses. In 2019, it was reported that the prevalence of HT was 19.7% in people over 15 years of age, being the male gender the most affected (21.7% vs. 17.8% in women), on the other hand, the prevalence of DM in people over 15 years of age was 3.9%, this time the female gender was more affected (4.3% vs. 3.4% in men).2
On the other hand, lifestyle is an important pillar in the prevention and treatment of NCDs. Mainly HT and DM include lifestyle modification in non-pharmacological treatment, especially in terms of exercise and diet. In addition, it is known that a healthy lifestyle reduces the number and doses of drugs used to manage these diseases and prevent future complications.3
On March 11, 2020, the WHO declared a pandemic due to the new SARS-COV 2 coronavirus.4In our country, the first infected person was confirmed on March 6, 2020, rapidly increasing the number of cases, presenting the first fatalities on March 19.5Therefore, a state of emergency was declared at the national level.6
The containment measures allowed the exclusive transit of “front line” personnel6, while the rest were forced to continue their work by virtual means. Likewise, the health centers focused on the care of patients with COVID-19, referring patients with CNCD to teleconsultations.
These changes in routine, increased stress, unemployment, social isolation, fear of being infected by COVID-19 when attending laboratories for routine examinations, and lack of access to their usual medications can generate negative behaviors in patients’ lifestyle and in the management of their diseases. On the contrary, the greater availability of time to spend with the family, cook healthily and carry out physical activity could improve the lifestyle and the control of these pathologies.7
As this issue is a worldwide concern, different countries conducted studies in the last year covering the other side of the COVID-19 pandemic, in this case, the impact that quarantine could have as a determining factor in the change in the style of life, eating habits, physical activity and routine disease control, in those patients with chronic non-communicable diseases.7-11In the context of the situation above, we set the following objective: To determine the association between lifestyle and the control of chronic non-communicable diseases: arterial hypertension and diabetes mellitus during the COVID-19 pandemic in patients from an Urgent Care Center.
METHODOLOGY
Type and design
An observational, cross-sectional, analytical, quantitative study was carried out in an emergency care center in Lima. The Urgent Care Center (CAU) - Emergency Control Unit (UCE), is a non-profit organization attended by patients with chronic diseases not related to COVID-19.
Population and Sample
This study includes all adult patients between 30 and 79 with arterial hypertension or diabetes mellitus who attended the CAU-UCE. Those patients who had only one chronic non-communicable disease were included: arterial hypertension or diabetes mellitus who had fasting blood pressure and glucose data on their control charts. Those with both diseases were excluded.
The sample size was determined using the finite population formula, for which the work of Samaneh Akbarpour, et al.12showing a total of 158 patients.
Statistical power of 80% and a confidence level of 95% were used. A non-probabilistic sampling was carried out because the study units have been selected for convenience, from the CAU-UCE, in the district of Lince.
Variables and instruments
The main variables were: lifestyle (independent variable) and control of arterial hypertension or diabetes mellitus (dependent variable).
To assess lifestyle, two types of questionnaires were used, the Lifestyle Profile of Nola Pender, in 1987 (PEPS I), adapted by Arrioja13in patients with arterial hypertension, which consists of 36 questions, showing a final score, where a score of 36 to 58 qualifies as unhealthy and from 59 to 144 as healthy. The general scale had Cronbach's Alpha 0.90, which is why it is considered acceptable.14Likewise, the questionnaire "Instrument to Measure the Lifestyle in Diabetics" (IMEVID) applied in patients with type 2 diabetes mellitus was used in a study carried out by Guzman and Ttupa, where a Cronbach's Alpha was obtained from 0.85 total instruments. (fifteen) This questionnaire consists of 25 questions, showing a final summation, where 0 to 74 points are considered unhealthy, and from 75 to 100 points is considered healthy.
To interpret and classify the results of the clinical variables related to the control of the disease in patients with HT and / or DM, the Ministry of Health's Clinical Practice Guide for the Diagnosis, Treatment and Control of hypertensive arterial disease and diabetes mellitus was used. Those who presented the last 6 blood pressure measurements <= 140/90 mmHg in the case of hypertensive patients were classified as “controlled patients”; and the last 2 fasting blood glucose measurements <= 130 mg / dL in the case of the diabetic patient.
Other variables studied were: age group, gender, marital status, educational level, length of illness, personal history of COVID-19, family history of COVID-19, and comorbidity. Likewise, during triage, the abdominal perimeter was measured, classifying the patient as normal risk (women <82cm, men <95 cm), high (women 82-87 cm, men 95-101 cm), and very high (women> 87 cm, males> 101 cm), height and weight were measured to obtain the calculation of the body mass index (BMI). The values were noted on the data collection form.
Procedures
Participation was openly voluntary, and written informed consent was requested from each participant who met the study’s inclusion criteria. The questionnaires were applied to the patients during the waiting time for their appointment in the general medical office, from 9:00 a.m. to 3:00 p.m., between October and November of 2020. Weight and height measurements were carried out, and abdominal girth using a smart scale and tape measures. Subsequently, the data collected was stored in a Microsoft Excel spreadsheet, where validation criteria were included to avoid possible typing errors.
Statistical Analysis
The quantitative variables were analyzed through measures of central tendencies, such as the mean. The measures of dispersion used to evaluate the frequency distribution of the variables were the mean and standard deviation when the distribution approached a normal one. For the qualitative variables, tables of frequencies and contingency were constructed.
To evaluate the association between the qualitative variables, the Chi-square test of independence was used. The prevalence ratio (PR) with its respective 95% condence interval was used to evaluate the association between lifestyle and disease control. Finally, the adjusted PRs were calculated through a Poisson regression model. The processing, recoding and validation, and statistical analysis were carried out in SPSS version 25.
Ethical Aspects
The present study was prepared to consider the ethical principles for medical research in human beings of the Declaration of Helsinki of the World Medical Association and its subsequent amendments. It was developed in the INICIB thesis degree course and had the approval of the Research Ethics Committee of the Faculty of Human Medicine of the Ricardo Palma University.
RESULTS
Of the total of 158 respondents, it is observed that 51.3% of the population is
made up of the male gender; 57.6% have a married marital status, and 51.9% have a higher educational level. Regarding the age of the patients, it is observed that the age was 39-79 years, the mean was 60.9 and with a standard deviation of 9.8. (Table 1)
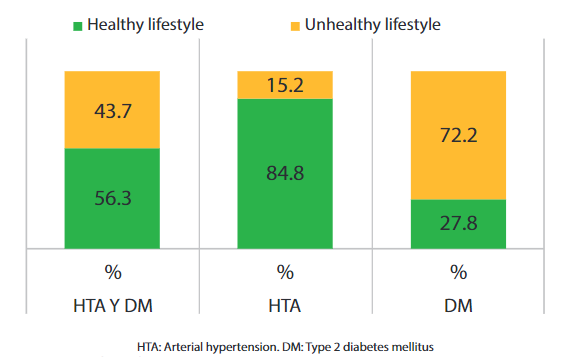
Control of the disease was reflected in 55.7% of the general population; It can also be shown that the majority of hypertensive patients have a healthy lifestyle (84.8%), in contrast to diabetic patients who have a higher percentage of an unhealthy lifestyle (72.2%). (Graph 1) With regard to BMI, overweight prevails in the population with 48.7% and an abdominal circumference with high risk in 36.7%. (Table 1)
Regarding comorbidities, 43.7% of the population does present some other disease, the most frequent being: dyslipidemia, osteoarthritis and migraine.
In the bivariate analysis of patients with arterial hypertension, it is evident that the variables that showed a significant association with the lack of control of the disease are: unhealthy lifestyle (PR = 3.190; p <0.001; 95% CI=2.233-4.558 ), Pathological BMI (PR=3.621; p=0.003; 95% CI=1.225-10.701), abdominal perimeter of pathological risk (PR=2.988; p=0.005; 95% CI=1.173-7.560) and family history of COVID-19 ( PR=2.094; p=0.011; 95% CI=1.321-3.319). (Table 2)
In the bivariate analysis of the population with type 2 diabetes mellitus, a significant association is shown between non-control of diabetes mellitus 2 and the following variables: unhealthy lifestyle (PR = 6.754; p <0.001; CI95 %=1.758-25.948), pathological BMI (PR=2.102; p=0.013; 95% CI=1.065-4.150), abdominal perimeter of pathological risk (PR=2.793; p=0.002; 95% CI=1.244-6.320) and time of disease older than 10 years (PR=0.584; p=0.030; 95% CI=0.350-0.977), the latter being a protective factor. (Table 3)
In the multivariate analysis of patients with arterial hypertension, a significant association between the lack of control of the hypertensive disease and an unhealthy lifestyle is evidenced (PR = 2.538; p = 0.000; 95% CI = 1.608-4.006). (Table 4) Finally, in the multivariate analysis of the diabetic population, a significant association was obtained between the non-control of diabetes mellitus with the following variables: unhealthy lifestyle (PR = 5.498; p = 0.013; 95% CI = 1.440 -20.995) and abdominal girth of pathological risk (PR = 2.623; p = 0.038; 95% CI = 1.057-6.508). (Table 5)
Table 1. General characteristics of the population in an Emergency Care Center, period October - December 2020.
| GENERAL CHARACTERISTICS | General | HTN | DM | ||||
| N° | % | N° | % | N° | % | ||
| Gender | Female | 81 | 51.3 | 34 | 43.0 | 43 | 54, 4 |
| Male | 77 | 48.7 | 45 | 57.0 | 36 | 45.6 | |
| Marital status | Single | 30 | 19.0 | 17 | 21.5 | 13 | 16.5 |
| Married | 91 | 57.6 | 42 | 53.2 | 49 | 62.0 | |
| Widowed | 11 | 7.0 | 6 | 7, 6 | 5 | 6.3 | |
| Divorced | 14 | 8.9 | 8 | 10.1 | 6 | 7.6 | |
| Cohabiting | 12 | 7.6 | 6 | 7.6 | 6 | 7.6 | |
| Educational level | University / Institute | 82 | 51.9 | 40 | 50.6 | 42 | 53.2 |
| High school | 65 | 41.1 | 35 | 44.3 | 30 | 38.0 | |
| Primary school | 11 | 7.0 | 4 | 5.1 | 7 | 8.9 | |
| Age Group | Adult | 75 | 47.5 | 38 | 48.1 | 37 | 46.8 |
| Older adult | 83 | 52.5 | 41 | 51, 9 | 42 | 53.2 | |
| Disease | control Controlled patient | 88 | 55.7 | 46 | 58.2 | 42 | 53.2 |
| patient Uncontrolled | 70 | 44.3 | 33 | 41.8 | 37 | 46.8 | |
| lifestyle | Healthy | 89 | 56.3 | 67 | 84.8 | 22 | 27.8 |
| Unhealthy | 69 | 43.7 | 12 | 15.2 | 57 | 72.2 | |
| Time of illness | Less than 10 years | 84 | 53.2 | 43 | 54.4 | 41 | 51.9 |
| More than 10 years | 74 | 46.8 | 36 | 45.6 | 38 | 48 , 1 | |
| Comorbidity | No | 89 | 56.3 | 40 | 50.6 | 49 | 62.0 |
| Yes | 69 | 43.7 | 39 | 49.4 | 30 | 38.0 | |
| BMI | Normal | 49 | 31.0 | 21 | 26.6 | 26 | 32.9 |
| Overweight | 77 | 48.7 | 43 | 54.4 | 36 | 45.6 | |
| Obesity grade I | 31 | 19.6 | 15 | 19.0 | 16 | 20.3 | |
| Obesity grade III | 1 | 0.6 | 0 | 0.0 | 1 | 1.3 | |
| Abdominal | circumference Normal risk | 47 | 29.7 | 23 | 29.1 | 24 | 30.4 |
| High risk | 58 | 36.7 | 29 | 36.7 | 29 | 36.7 | |
| Very high risk | 53 | 33, 5 | 27 | 34.2 | 26 | 32.9 | |
| History of COVID-19 | No | 137 | 86.7 | 71 | 89.9 | 66 | 83.5 |
| Yes | 21 | 13.3 | 8 | 10.1 | 13 | 16.5 | |
| Family history of COVID-19 | No | 128 | 81, 0 | 67 | 84.8 | 61 | 77.2 |
| Yes | 30 | 19.0 | 12 | 15.2 | 18 | 22.8 | |
| Total | 158 | 100 | 79 | 50 | 79 | 50 | |
HT: Arterial hypertension. DM: Type 2 diabetes mellitus. BMI: Body mass index
Table 2. Bivariate analysis of the population with arterial hypertension at the Emergency Care Center, October - December 2020
| GENERAL CHARACTERISTICS | DISEASE CONTROL | |||||||||||
| Total | Patient Uncontrolled | Patient controlled | Chi square | P value | PR | CI 95% | ||||||
| Total | 79 (100%) | 33 (41,8%) | 46 (58,2%) | |||||||||
| Lifestyle | Unhealthy | 12 (100%) | 12 (100%) | 0 (0%) | 19,723 | 0,000* | 3,190 | 2,233-4,558 | ||||
| Healthy | 67 (100%) | 21 (31,34%) | 46 (68,66%) | Ref. | Ref. | Ref. | Ref. | |||||
| Age group | Older adult | 41 (100%) | 14 (34,15%) | 27 (65,85%) | 2,038 | 0,153 | 0,683 | 0,400-1,165 | ||||
| Adult | 38 (100%) | 19 (50%) | 19 (50%) | Ref. | Ref. | Ref. | Ref. | |||||
| Gender | Female | 34 (100%) | 15 (44,12%) | 19 (55,88%) | 0,135 | 0,713 | 1,103 | 0,653-1,863 | ||||
| Male | 45 (100%) | 18 (40%) | 27 (60%) | Ref. | Ref. | Ref. | Ref. | |||||
| Status | With partner | 48 (100%) | 22 (45,83%) | 26 (54,17%) | 0,8295 | 0,362 | 1,292 | 0,731-2,282 | ||||
| No partner | 31 (100%) | 11 (35,48%) | 20 (64,52%) | Ref. | Ref. | Ref. | Ref. | |||||
| educational level | College | 39 (100%) | 20 (51,28%) | 19 (48,72%) | 2,864 | 0,091 | 1,578 | 0,915-2,721 | ||||
| Superior | 40 (100%) | 13 (32,50%) | 27 (67,50%) | Ref. | Ref. | Ref. | Ref. | |||||
| Time of illness | More than 10 years | 36 (100%) | 15 (41,67%) | 21 (58,23%) | 0,000 | 0,986 | 0,995 | 0,588-1,685 | ||||
| Less than 10 years | 43 (100%) | 18 (41,86%) | 25 (58,14%) | Ref. | Ref. | Ref. | Ref. | |||||
| BMI | Pathological | 58 (100%) | 30 (51,72%) | 28 (48,28%) | 8,885 | 0,003 | 3,621 | 1,225-10,701 | ||||
| Normal | 21 (100%) | 3 (14,29%) | 18 (85,71%) | Ref. | Ref. | Ref. | Ref. | |||||
| Abdominal | circumference Pathological risk | 56 (100%) | 29 (51,79%) | 27 (48,21%) | 79,295 | 0,005 | 2,978 | 1,173-7,560 | ||||
| Normal risk | 23 (100%) | 4 (17,39%) | 19 (82,61%) | Ref. | Ref. | Ref. | Ref. | |||||
| Personal history of COVID-19 | Yes | 8 (100%) | 5 (62,50%) | 3 (37,50%) | 1,572 | 0,210 | 1,585 | 0,858-2,926 | ||||
| No | 71 (100%) | 28 (39,44%) | 43 (60,56%) | Ref. | Ref. | Ref. | Ref. | |||||
| family members of COVID-19 | Yes | 12 (100%) | 9 (75%) | 3 (25%) | 6,423 | 0,011 | 2,094 | 1,321-3,319 | ||||
| No | 67 (100%) | 24 (35,82 %) | 43 (64,18%) | Ref. | Ref. | Ref. | Ref. | |||||
| comorbidity | Yes | 39 (100%) | 19 (48,72%) | 20 (51,28%) | 1,528 | 0,216 | 1,392 | 0,816-2,375 | ||||
| No | 40 (100%) | 14 (35%) | 26 (65%) | Ref. | Ref. | Ref. | Ref. | |||||
* Fisher's exact probability test between disease control and lifestyle in patients with HTN at the Urgent Care Center, October - December 2020 period.
Table 3. Bivariate analysis of the population with diabetes Type 2 Mellitus P-value Chi-square patient in the Emergency Care Center, October - December period September 2020.
| GENERAL CHARACTERISTICS | DISEASE CONTROL | ||||||||||
| Total | Patient Uncontrolled | Patient controlled | Chi square | P value | PR | CI 95% | |||||
| Total | 79 (100%) | 37 (48,8%) | 42 (53,2%) | ||||||||
| lifestyle | No healthy | 57 (100%) | 35 (61,40%) | 22 (38,60%) | 17,446 | 0,000 | 6,754 | 1,758-25,948 | |||
| Healthy | 22 (100%) | 2 (9,09%) | 20 (90,91%) | Ref. | Ref. | Ref. | Ref. | ||||
| Age group | Senior | 42 (100%) | 19 (45,24%) | 23 (54,76%) | 0,092 | 0,762 | 0,9298 | 0,5798-1,491 | |||
| Adult | 37 (100%) | 18 (48,65%) | 19 (51,35%) | Ref. | Ref. | Ref. | Ref. | ||||
| Gender | Female | 43 (100%) | 18 (41,86%) | 25 (58,14%) | 0,938 | 0,333 | 0,793 | 0,495-1,271 | |||
| Male | 36 (100%) | 19 (52,78%) | 17 (47,22%) | Ref. | Ref. | Ref. | Ref. | ||||
| Marital status | With partner | 55 (100%) | 27 (49,09%) | 28 (50,91%) | 0.369 | 0,543 | 1,178 | 0,681-2,038 | |||
| Without partner | 24 (100%) | 10 (41,67%) | 14 (58,33%) | Ref. | Ref. | Ref. | Ref. | ||||
| Educational level | School | 37 (100%) | 19 (51,35%) | 18 (48,65%) | 0.57 | 0,450 | 1,198 | 0,747-1,921 | |||
| Superior | 42 (100%) | 18 (42,86%) | 24 (57,14%) | Ref. | Ref. | Ref. | Ref. | ||||
| Time disease | Over 10 years | 38 (100%) | 13 (34,21%) | 25 (65,79%) | 4,687 | 0,030 | 0,584 | 0,350-0,977 | |||
| Less than 10 years | 41 (100%) | 24 (58,54%) | 17 (41,46%) | Ref. | Ref. | Ref. | Ref. | ||||
| BMI | Pathological | 53 (100%) | 30 (56,60%) | 23 (43,40%) | 6,171 | 0,013 | 2,102 | 1,065-4,150 | |||
| Normal | 26 (100%) | 7 (26,92%) | 19 (73,08%) | Ref. | Ref. | Ref. | Ref. | ||||
| Abdominal | circumference Pathological risk | 55 (100%) | 32 (58,18%) | 23 (41,82%) | 9,360 | 0,002 | 2,793 | 1,234-6,320 | |||
| Normal risk | 24 (100%) | 5 (20,83%) | 19 (79,17%) | Ref. | Ref. | Ref. | Ref. | ||||
| Personal history of COVID-19 | Yes | 13 (100%) | 6 (46,15%) | 7 (53,85%) | 0,003 | 0,957 | 0,983 | 0,516-1,872 | |||
| No | 66 (100%) | 31 (46,97%) | 35 (53,03%) | Ref. | Ref. | Ref. | Ref. | ||||
| Family history of COVID-19 | Yes | 18 (100%) | 8 (44,44%) | 10 (55,56%) | 0,054 | 0,817 | 0,935 | 1,676-0,620 | |||
| No | 61 (100%) | 29 (47,54%) | 32(52,46%) | Ref. | Ref. | Ref. | Ref. | ||||
| Comorbidity | Yes | 30 (100%) | 13 (43,33%) | 17 (56,67%) | 0,238 | 0,625 | 0,885 | 0,535-1,462 | |||
| No | 49 (100%) | 24 (48,98%) | 25 (51,02%) | Ref. | Ref. | Ref. | Ref. | ||||
BMI: Body mass index
Table 4. Multivariate analysis of patients with arterial hypertension in the Emergency Care Center, October - December 2020.
| GENERAL CHARACTERISTICS ARTERIAL | HYPERTENSION | ||||
| P-value | RP adjusted | 95% IC | |||
| Lower | Upper | ||||
| Lifestyle | No healthy | 0,000 | 2,538 | 1,608 | 4,006 |
| Healthy | 1 | ||||
| BMI | Pathological | 0,240 | 2,270 | 0,578 | 8,912 |
| Normal | 1 | ||||
| waist circumference | Pathological | 0,451 | 1,581 | 0,480 | 5,206 |
| Normal | 1 | ||||
| Family history of covid-19 | Yes | 0,916 | 1,025 | 0,653 | 1,607 |
| No | 1 | ||||
BMI: Body mass index
Table 5. Multivariate analysis of patients with type 2 diabetes mellitus in the Emergency Care Center, October - December 2020.
| GENERAL CHARACTERISTICS | DIABETES MELLITUS | |||||
|---|---|---|---|---|---|---|
| P-value | Adjusted RP | 95% CI | ||||
| Lower | Upper | |||||
| Style of living | Unhealthy | 0,013 | 5,498 | 1,440 | 20,995 | |
| healthy | 1 | |||||
| BMI | Pathological | 0,491 | 0,778 | 0,380 | 1,592 | |
| Normal | 1 | |||||
| Abdominal | Pathological | 0,038 | 2,623 | 1,057 | 6,508 | |
| Normal | 1 | |||||
| TLength of illness | More than 10 years | 0,096 | 0,677 | 0,428 | 1,071 | |
| Less than 10 years | 1 | |||||
BMI: Body mass index
DISCUSSION
In the present study, a significant association between unhealthy lifestyle and non-control of HT and DM2 was determined in patients who attended the Emergency Care Center - UCE, during the COVID-19 pandemic. Within the population with arterial hypertension, the prevalence of non-control of NCD was 1.5 times more in patients with an unhealthy lifestyle than those with a healthy lifestyle (PR = 2.538; p = 0.000; 95% CI = 1.608-4.006). A study carried out by Hernández et al., in Mexico, in 306 hypertensive patients obtained similar results. They concluded that there is a significant association between lifestyle and control of hypertension, demonstrating that patients with worse lifestyles do not present control of disease (p = 0.0001).16Yokokawa et al, in a study conducted in Japan in hypertensive patients, revealed that maintaining a healthy lifestyle was a significant protective factor to in achieving target blood pressure: <140 /90 mmHg (OR=.51; 95% CI=0.36-0.72).17
In the present investigation, it was obtained that the population of patients with type 2 diabetes mellitus shows a significant association between an unhealthy lifestyle and the lack of control of the diabetic disease (PR = 5.498; p = 0.013; 95% CI = 1,440-20,995). In a study similar to ours, carried out in Cajamarca by Asenjo, in a total of 102 patients with DM2, it was concluded that there is a direct and significant relationship between lifestyle and metabolic control (p <0.001).18Likewise, the study carried out by Vásquez et al. In Mexico, a sample of 330 patients with DM2 was taken, it was found that a good lifestyle is a protective factor for glycemic control (OR = 0.026; p = 0.001; 95% CI = 0.009-0.077), unlike our study In this, HbA1c <7% was used as a glycemic control parameter.19
In the context of conducting this study in the midst of a pandemic in conjunction with those described above, Mattioli et al. emphasize that the change in lifestyle and routine activities are consequences of stress related to confinement, which includes changes in nutritional habits, which may be due to less availability of products in the market, limited access to stores due to changes in their opening hours and the preference for unhealthy foods (processed foods, packaged foods) for their longer duration, as the large amounts of salt, sugar or trans fats they contain increase their life span useful.11
It is known that confinement generates high levels of stress, which affects the balance in the sympathetic-parasympathetic nervous system and the hypothalamic-pituitary-adrenal axis, causing direct cardio-stimulatory effects (positive chronotrope and inotrope), vasopressor effects, increased insulin resistance, increased lipolysis and acceleration of the atherosclerotic process, negatively affecting the cardiovascular and metabolic system.11Likewise, Laura Di Renzo et al., in their study carried out on 3,533 people in Italy, observed that 37.3% of the population had modifications in their lifestyle and eating habits during the quarantine pandemic by COVID-19, where 16.7% made positive modifications.8In the same way, in the study by Cancello et al, carried out in northern Italy, in a sample of 490 adults, it is concluded that more than a third of the people were able to make a positive change in their styles life during home quarantine7. In contrast to this, Muhammad's study applied to 181 participants in Pakistan shows that 45% of the population had a negative effect on their health, pointing out certain challenges due to quarantine: difficulty exercising (66%), missing to their routine check-ups (53%) and to miss their regular laboratory tests (42%).9This would be consistent with a study carried out virtually by Chudasama on 202 health professionals in 47 different countries, most of them belonging to the European continent (47%), where it is evidenced that most of the patients had a negative impact on the routine care of their chronic diseases since the beginning of the pandemic (46%), and 47.8% of the population was affected by the shortage of medicines; also reports that diabetes and arterial hypertension (30%) were the two comorbidities for which care was most affected in this quarantine period.10
Likewise, the present study shows that in the population with type 2 diabetes mellitus, the abdominal girth of pathological risk and glycemic lack of control were shown to have a significant association (p = 0.038), with a prevalence of non-control of the disease of 1.6 times more in those patients with pathological risk abdominal girth compared to patients with normal abdominal girth (OR = 2.623; 95% CI = 1.057-6.508). It is known that multiple factors intervene in the control of the disease, one of the most studied is the anthropometric values (BMI and abdominal circumference). Obesity (BMI> 30) is considered a pro-inflammatory state; Likewise, the increased abdominal girth is considered a marker of insulin resistance. Both parameters are usually associated with poor control of the disease in patients with HT and DM2. Pérez et al, in their study carried out in Spain in 5591 patients with DM2, found that the time of evolution of the disease <10 years (OR=1.385; p <0.0001; 95% CI=1.21-1.586), the absence of dyslipidemia and abdominal girth in normal values (OR=1.410; p <0.001; 95% CI=1.187-1.675) are factors associated with adequate glycemic control20. On the other hand, Vásquez et al., evidence in their study that the increase in BMI is significantly associated with the increased risk of glycemic uncontrol in patients with DM2 (OR = 2.70; p = 0.001; 95% CI = 2.00- 3.65).19
In the present study, the history of COVID-19 is divided into two categories, one indicates the personal history of having had the disease, and the other indicates the history that a relative who lives with the patient presented the disease. According to this, it is evident that there is no significant association between this variable and the control of the disease. It is known that those people who suffer from CNCD and become infected with COVID-19 have a high probability of progressing to severe disease, with a significant increase in mortality, with arterial hypertension and diabetes mellitus being the most frequent comorbidities in patients hospitalized for COVID-19.
CONCLUSIONS
A healthy lifestyle is significantly associated with the control of arterial hypertension and also with type 2 diabetes mellitus in adult patients during the COVID-19 pandemic. On the other hand, non-control of diabetes mellitus is 1.6 times more prevalent in diabetic patients with abnormal abdominal girth than in diabetic patients with normal abdominal girth. Finally, the sociodemographic factors (age group, gender, marital status, educational level) did not significantly affect hypertension and DM2.
Acknowledgments:
REFERENCES
1. Palomino EEB. Prevalencia de factores de riesgo para enfermedades crónicas no transmisibles en Perú. Rev Cuid. 2020;11(2):5-5. DOI: https://doi.org/10.15649/cuidarte.1066 [ Links ]
2. Programas de Enfermedades No Trasmisibles [Internet]. [citado 30 de septiembre de 2020]. Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1734/cap01.pdf [ Links ]
3. Araya-Orozco M. Hipertensión arterial y diabetes mellitus. Rev Costarric Cienc Médicas. 2004;25(3-4):65-71. Disponible en: https://www.scielo.sa.cr/scielo.php?script=sci_arttext&pid=S0253-29482004000200007 [ Links ]
4. La OMS caracteriza a COVID-19 como una pandemia - OPS/OMS | Organización Panamericana de la Salud [Internet]. [citado 1 de octubre de 2020]. Disponible en: http://www.paho.org/es/noticias/11-3-2020-oms-caracteriza-covid-19-como-pandemia [ Links ]
5. Características Clinicoepidemiológicas de pacientes fallecidos por COVID-19 en un Hospital Nacional de Lima, Perú [Internet]. [citado 1 de abril de 2021]. Disponible en: http://www.scielo.org.pe/scielo.php?pid=S2308-05312020000200180&script=sci_arttext [ Links ]
6. Decreto Supremo N° 044-2020-PCM [Internet]. [citado 1 de octubre de 2020]. Disponible en: https://www.gob.pe/institucion/pcm/normas-legales/460472-044-2020-pcm [ Links ]
7. Cancello R, Soranna D, Zambra G, Zambon A, Invitti C. Determinants of the Lifestyle Changes during COVID-19 Pandemic in the Residents of Northern Italy. Int J Environ Res Public Health. 2020;17(17):6287. DOI: 10.3390/ijerph17176287 [ Links ]
8. Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attinà A, Cinelli G, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):229. DOI: https://doi.org/10.1186/s12967-020-02399-5 [ Links ]
9. Saqib MAN, Siddiqui S, Qasim M, Jamil MA, Rafique I, Awan UA, et al. Effect of COVID-19 lockdown on patients with chronic diseases. Diabetes Metab Syndr Clin Res Rev. 2020;14(6):1621-3. DOI: 10.1016/j.dsx.2020.08.028 [ Links ]
10. Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, et al. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14(5):965-7. DOI: 10.1016/j.dsx.2020.06.042 [ Links ]
11. Mattioli AV, Sciomer S, Cocchi C, Maffei S, Gallina S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr Metab Cardiovasc Dis. 2020;30(9):1409-17. DOI: 10.1016/j.numecd.2020.05.020 [ Links ]
12. Akbarpour S, Khalili D, Zeraati H, Mansournia MA, Ramezankhani A, Fotouhi A. Healthy lifestyle behaviors and control of hypertension among adult hypertensive patients. Sci Rep. 2018;8(1):8508. DOI: https://doi.org/10.1038/s41598-018-26823-5 [ Links ]
13. Arrioja Morales G. Estilo de vida en el paciente con hipertensión arterial. Tesis de maestría. Universidad Autónoma de Nuevo León, 2001. Disponible en: http://eprints.uanl.mx/6182/ [ Links ]
14. Zela Ari L, Mamani Chambi W, Mamani Limachi RE. Hipertensión arterial y estilo de vida en adultos mayores de la Micro Red de Salud Revolución San Román, Juliaca - 2015. Revista de Investigación Universitaria 2015;4:35-41. DOI: https://doi.org/10.17162/riu.v4i1.609. [ Links ]
15. Guzmán Ramos JY, Ttupa Tucno NA. Estilos de vida de los pacientes con Diabetes Mellitus tipo II que asisten al Programa de Diabetes del Hospital Nacional Dos de Mayo, Lima - 2016. Univ Nac Callao [Internet]. 2016 [citado 1 de abril de 2021]; Disponible en: http://repositorio.unac.edu.pe/handle/UNAC/1777 [ Links ]
16. Hernández de la Rosa M, Godoy Quinto J, Romero San Salvador CY, Gutiérrez Gabriel I, Arthur Aguirre F. Efecto del estilo de vida en el control de pacientes con hipertensión arterial sistémica en una unidad de medicina familiar en Puebla, México. Aten Fam. 2018;25(4):155. DOI: http://dx.doi.org/10.22201/facmed.14058871p.2018.4.67260 [ Links ]
17. Yokokawa H, Goto A, Sanada H, Watanabe T, Felder RA, Jose PA, et al. Association between control to target blood pressures and healthy lifestyle factors among Japanese hypertensive patients: Longitudinal data analysis from Fukushima Research of Hypertension (FRESH). Obes Res Clin Pract. 2014;8(4):e364-73. DOI: 10.1016/j.orcp.2013.08.004 [ Links ]
18. Asenjo-Alarcón JA, Asenjo-Alarcón JA. Relación entre estilo de vida y control metabólico en pacientes con Diabetes Mellitus Tipo 2 de Chota, Perú. Rev Medica Hered. 2020;31(2):101-7. DOI: http://dx.doi.org/10.20453/rmh.v31i2.3771 [ Links ]
19. Vásquez Arroyo SB, Roy García IA, Velázquez López L, Navarro Susano LG. Impacto del estilo de vida en el descontrol glucémico en pacientes con diabetes mellitus tipo 2. Aten Fam. 2018;26(1):18-22. DOI: http://dx.doi.org/10.22201/facmed.14058871p.2019.1.67712 [ Links ]
20. Pérez A, Mediavilla JJ, Miñambres I, González-Segura D. Control glucémico en pacientes con diabetes mellitus tipo 2 en España. Rev Clínica Esp. 2014;214(8):429-36. DOI: https://doi.org/10.1016/j.rce.2014.05.028 [ Links ]
Received: March 19, 2021; Accepted: July 09, 2021











 texto en
texto en