Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.3 Lima jul./set. 2022 Epub 09-Jul-2022
http://dx.doi.org/10.25176/rfmh.v22i3.4744
Original Article
Relationship between food frequency and schedule with overweight and obesity
1Faculty of Medicine. National University of Trujillo. Trujillo, Peru.
Introduction:
Overweight and obesity present rapid growth in the world, with an increased risk of chronic diseases. Nutritional strategies are of great interest for weight control and loss, as is the influence of feeding frequency and schedule.
Objective:
To determine the relationship between feeding frequency and schedule with overweight and obesity in the Trujilloan adult population aged 30 to 70.
Methods:
Descriptive, cross-sectional study with a quantitative approach. A sample of 160 participants aged between 30 and 70 years was included; the data were collected through a virtual survey. Participants were classified into a normal weight group established by BMI between 18.5-24.9 and an overweight-obesity group established by BMI greater than or equal to 25. An expert-validated questionnaire was used to assess feeding frequency and schedule.
Results:
Of the 160 participants, 61.88% were of the female sex, and 40% had aged between 30-39 years. The normal weight group was conformed of 60 participants, and the overweight obesity consisted of overweight-obesity per 100 participants. In the statistical analysis, a significant difference was evidenced between the low-moderate physical activity level (p=0.019), the feeding frequency presented no significant difference (p=0.477), and within the feeding schedule, the post-dinner consumption at 8:00 pm presented a significant difference (p=0.021), as well as the consumption of intermediates after 5:00 pm (p=0.016).
Conclusion:
Consume food during the evening at a time after 8:00 pm is significantly associated with risk of overweight and obesity; while at the feed frequency it is not presented.
Keywords: Food intake; Overweight; Obesity. (fuente: MeSH NLM).
INTRODUCTION
Obesity is a rapidly growing worldwide epidemic; its prevalence has nearly doubled in more than 70 countries since 19801. 75% of the world population lives in countries where overweight and obesity are responsible for higher mortality compared to underweight1; this is due to its negative impact on health which is associated with an increased risk of developing chronic diseases, such as type II diabetes, cardiovascular diseases, musculoskeletal disorders and some cancers2.
In Peru, the Report “Peru: Non-communicable and communicable diseases”, where the Body Mass Index (BMI) was assessed in people aged 15 years and older, showed that in 2019, the prevalence of overweight and obesity was 37.8% and 22.3%, respectively3. Comparing these figures with 2013, an increase of 4.0 percentage points is observed in both conditions.
Before that, within the proposed strategies to reduce energy intake (diets, drugs, and bariatric surgery) and increase energy production (exercise and movement without exercise), the schedule and frequency of meals could exert a significant influence on the control and weight loss1,4.
Interestingly, the relationship between feeding frequency and changes in BMI is still controversial. In some research, eating one or two meals daily was associated with a relatively lower BMI compared with three meals daily; while in others a negative relationship was found between feeding episodes and the prevalence of abdominal obesity1,5.
On the other hand, regarding the timing of meals, it has been suggested that eating later in the evening may negatively influence the success of a weight loss therapy6. It has also been observed that regular ingesting food in the morning can protect against weight gain by reducing absolute energy intake during the day(7). This difference between early versus late feeding has been related to the internal circadian clock1,7-9.
Precisely, through the circadian clock system, it is explained why the feeding schedule has an impact on body weight regulation; since it is involved in metabolic rhythms, including glucose and lipids9. According to research, the organism's capacity to assimilate carbohydrates is highest in the morning, and the activity of adipocytes in lipid metabolism decreases in the evening10,11. This leads to our body processing food more slowly and converting it into fats more easily during the night than in the morning.
For this reason, the present research seeks to contribute knowledge about the topic in the concrete reality of the adult Trujillo population to avoid the potential increase in overweight and obesity due to the negative health consequences they bring.
METHODS
Design and study area
An analytical, cross-sectional study with a quantitative approach was conducted.
Population and sample
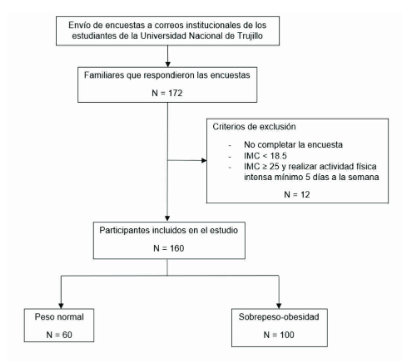
The population was conformed of the family members of the students of the Universidad Nacional de Trujillo. All those presenting residences in the province of Trujillo, of both sexes and aged between 30 and 70 years were included; the exclusion criteria were not completing the survey, presenting underweight established as BMI < 18.5, loss of any limb and participants with a BMI equal to or greater than 25 who performed intense physical activity a minimum of 5 days a week. The sample was confirmed by 160 participants by non-probability sampling by convenience.
Variables and instruments
The independent variables were feeding frequency, defined as the number of main (breakfast, lunch, and dinner) and intermediate meals (foods or beverages consumed between main meals) ingested during the day; and the feeding schedule, defined as the hours during the day during which food is ingested, in which breakfast intake was considered as before 6:00 am until 9:59 am; lunch, from 12:00 pm to 5:59 pm; dinner, from 7:00 pm until after 9:00 pm; and the intervals which were split into two schedules, during the morning from 8:00 am to 11:59 am and during the afternoon-night from 3:00 pm until after 9:00 pm. The dependent variable was overweight-obesity which was set as a BMI greater than or equal to 25. Likewise, daily sleep hours and physical activity were considered intervening variables.
To assess feeding frequency and schedule, a questionnaire was developed by the present study's authors and validated by five nutrition and research experts from the Universidad Nacional de Trujillo.
On the other hand, overweight-obesity was assessed by the BMI, which was calculated according to Quetelet’s formula weight(kg) / [height(m)]2 based on the data provided by the participants. To assess the intervening variables, the IPAQ test was used for the level of physical activity. Daily sleep hours were evaluated with the indicators less than 5 hours, between 5 and 8 hours, and more than 8 hours. All this was contemplated in the online survey crafted through the Google Forms platform.
Procedures
The data collection took place between December 2021 and January 2022. For obtaining the data an online survey was used by the Google Forms platform, which was sent through the institutional mails of the students of the National University of Trujillo. A total of 172 responses were obtained, of which 12 were excluded for not completing the survey, for presenting underweight (BMI < 18.5) or for having a BMI equal to or greater than 25 and performing intense physical activity a minimum of 5 days a week; remaining a total of 160 participants.
Subsequently, the 160 participants were classified into a normal weight group established by a BMI between 18.5-24.9 and an overweight-obesity group established by a BMI greater than or equal to 25. In the normal weight group, a total of was obtained 60 participants
Statistical analysis
For the analysis, a database designed in the program Microsoft Excel 2016 was used. Through the same program, frequency and contingency tables were constructed, and the association between variables was evaluated by Chi-square hypothesis testing with a level of significance p < 0.05.
Ethical aspects
The present study elaborated on respecting the ethical principles of the Declaration of Helsinki for research on human beings. Acceptance of informed consent by the participants at the beginning of the questionnaire was considered as well as, and no data collected allowed the identification of the participants. The work was approved by the Research Ethics Committee of the Faculty of Medicine of the National University of Trujillo.
RESULTS
The participants were classified according to sex and age group (Table 1), 99 were females and 61 males. A similar proportion of females and males was observed in both groups. Participants between 30 - 39 years old represented a higher percentage in the normal weight group and in the overweight-obesity one.
Table 1. Sociodemographic characteristics of the normal weight and overweight-obese groups.
| VARIABLE | NORMAL WEIGHT | OBESITY | TOTAL | p | |||
| N=60 | % | N=100 | % | ||||
| Sex | Female | 36 | 60.00 | 63 | 63.00 | 99 | 0.70 |
| Male | 24 | 40.00 | 37 | 37.00 | 61 | ||
| Age | 30-39 years | 29 | 48.30 | 35 | 35.00 | 64 | 0.20 |
| 40-49 years | 13 | 21.70 | 32 | 32.00 | 45 | ||
| 50-70 years | 18 | 30.00 | 33 | 33.00 | 51 | ||
Overweight-obesity persons had a higher frequency of low-moderate physical activity (Table 2), statistically significant.
Table 2. Physical activity level according to the IPAQ test and hours of daily sleep in the normal-weight and overweight-obese groups.
| VARIABLE | NORMAL WEIGHT | OBESITY | TOTAL | p | ||||
| N=60 | % | N=100 | % | |||||
| Physical activity level | ||||||||
| Low-Moderate | 33 | 55.00 | 73 | 73.00 | 106 | 0.019 | ||
| High | 27 | 45.00 | 27 | 27.00 | 54 | |||
| Hours of sleep | ||||||||
| Less than 5 hours | 8 | 13.33 | 11 | 11.00 | 19 | 0.722 | ||
| 5 to 8 hours | 48 | 80.00 | 79 | 79.00 | 127 | |||
| More than 8 hours | 4 | 6.67 | 10 | 10.00 | 14 | |||
The number of sleep hours were similar in both groups (Table 2). , is from 5 to 8 hours of daily sleep most common.
The frequency of food consumption presented no significant difference (Table 3), the usual number of daily meals both in the normal weight and the overweight-obese group was 3 meals or less.
Table 3. Feeding frequency in the normal weight and overweight groups.
| FREQUENCY OF FEEDING | NORMAL WEIGHT | OBESITY | TOTAL | p | ||||
| N=60 | % | N=100 | % | |||||
| 3 times or less | 35 | 58.33 | 58 | 58.00 | 85 | 0.477 | ||
| 4 times | 18 | 30.00 | 24 | 24.00 | 42 | |||
| 5 times or more | 7 | 11.00. 67 | 18 | 18,00 | 25 | |||
The normal weight and the overweight-obese group consumed breakfast most frequently in the 8:00-9:59 am schedule; and lunch, from 12:00-1:59 p.m. The overweight-obesity group consumed dinner and late-evening interludes on a later schedule than the normal weight group, with significant differences (Table 4).
Table 4. Feeding schedule in the normal weight and overweight-
| SCHEDULE OVERWEIGHT | NORMAL WEIGHT | -OBESE | TOTAL | p | |||||
| N=60 | % | N=100 | % | ||||||
| Breakfast | Before 8:00 am | 21 | 35.00 | 25 | . 00 | 46 | 0.143 | ||
| 8:00-9:59 am | 32 | 53.33 | 52 | 52.00 | 84 | ||||
| No set hours or no breakfast | 7 | 11.67 | 23 | 23.00 | 30 | ||||
| Lunch | 12:00-1:59 pm | 33 | 55.00 | 48 | 48.00 | 81 | 0.651 | ||
| After 2:00 pm | 22 | 36.67 | 44 | 44.00 | 66 | ||||
| Has no set hours or no lunch | 5 | 8.33 | 8 | 8.00 | 13 | ||||
| Dinner | 7:00-7:59 pm | 24 | 40.00 | 20 | 20.00 | 44 | 0.021 | ||
| After 8:00 pm | 27 | 45.00 | 57 | 57.00 | 74 | ||||
| Has no fixed schedule or no dinner | 9 | 15.00 | 23 | 23.00 | 32 | ||||
| 00-10 Morning | :59 am | 22 | 36 ,67 | 48 | 48.00 | 70 | 0.21 | ||
| After 11:00 am | 15 | 25.00 | 15 | 15.00 | 30 | ||||
| Does not consume | 23 | 38.33 | 37 | 37.00 | 60 | ||||
| Late -evening | intervals 3:00-4:59 pm | 15 | 25.00 | 9 | 9.00 | 24 | 0.016 | ||
| After 5:00 pm | 26 | 43.33 | 45 | 45.00 | 71 | ||||
| Does not consume | 19 | 31.67 | 46 | 46.00 | 65 | ||||
DISCUSSION
In the present research a significant relationship was found between the consumption of late dinner during the n oche (after 8:00 pm) with overweight and obesity, these findings are similar to those found by Ha K, et al.6where they observed an increase in the prevalence of obesity and metabolic syndrome associated with eating after 9:00 pm in Korean adults. Also, it was found that the consumption of intermediates during the late evening in the overweight and obese group was significantly later than that of normal weight, which was not evidenced with the intermediates during the morning. These findings are consistent with Barrington W, et al.12, who found an association between intermediate evening consumption with obesogenic behavior but not with morning or midday intermediates.
Based on this, it is deduced that overweight or obese people consume food during the night at a later schedule than normal weight people. This coincides with that reported by Xiao, et al.7; Yoshida, et al.13; Kutsuma, et al.,14and Berg, et al.15; who pointed out that people with nocturnal eating habits such as eating dinner immediately before bedtime or consuming “snacks” after dinner, have higher odds of developing obesity than those who don’t present these habits.
No significant difference in breakfast schedule was found between the normal weight and overweight or obese groups, as well as between those who did eat breakfast and those who did not. However, studies indicate that not consuming breakfast has been associated with an increased risk of overweight and obesity; as reported by Guinter M, et al.16, where women who ate breakfast 7 days a week presented a decreased risk of overweight and obesity, compared with women who ate breakfast 3 to 4 days a week. Odegaard A, et al.17found that people who ate breakfast 3 days a week or less had a risk of obesity 1.33 times higher than people who ate breakfast 4 to 6 days a week and 1.75 times higher than those who ate breakfast 7 days to the week. Goto M, et al.18evidenced that it was 1.34 times more likely a >5 % increase in BMI value in men who did not eat breakfast 2 or more days a week compared to those who did not eat breakfast only 1 day a week or less than.
The frequency of food consumption in normal weight and overweight-obese individuals did not evidence significant differences, being in both groups habitual consumption of 4 to less meals daily. This contrasts with the findings of Ha K, et al.6and Holmbäck I, et al.19that indicate an association between a higher number of feeding episodes with a lower prevalence of abdominal obesity. Similarly, Aljuraiban G, et al.20found that participants who ate 6 or more meals a day compared to those who ate less than 4 meals had a lower BMI. However, Van der Heijden A, et al.21observed that an increase in feeding frequency beyond 3 daily meals was associated with an increased risk of weight gain of 5 kg at 10 years. Additional studies are needed to better understand the role of meal frequency in overweight and obesity risk.
Also, physical activity and hours of daily sleep were considered as intervening variables. Regarding low-moderate physical activity, this predominated in overweight or obese participants than in those with a normal weight. This finding was significant and similar to the work of Xiao, et al.7who found a lower level of physical activity determined by the number of steps per day in overweight-obese participants.
Sleep hours can influence people’s weight, as noted by Canuto R, et al.22who found obesity prevalence ratios of 1.4 and 4.4 in workers with sleep deprivation at levels I (<5 h of continuous sleep/day with some additional rest) and II (<5 h of sleep continuous/day without additional rest), respectively. This effect was not found in the present study.
Within the limitations of the paper, it can be pointed out that the number could be higher to obtain significant results. The weight and height data were self-reported, due to reasons virtuality could not be done face-to-face. In addition, the study is cross-sectional analytic so causality cannot be assessed; likewise, the sampling was non-probabilistic, which causes a loss of representativeness.
REFERENCES
1. Paoli A, Tinsley G, Bianco A, Moro T. La influencia de la frecuencia y el momento de las comidas en la salud de los seres humanos: el papel del ayuno. Nutrientes. 2019; 11 (4): 719. DOI: 10.3390/nu11040719. [ Links ]
2. Harris L, Hamilton S, Azevedo LB, Olajide J, De Brún C, Waller G, et al. Intervenciones de ayuno intermitente para el tratamiento del sobrepeso y la obesidad en adultos: una revisión sistemática y metaanálisis. Informe de implementación del sistema de base de datos del JBI. 2018; 16 (2): 507-547. doi: 10.11124/JBISRIR-2016-003248. [ Links ]
3. Instituto Nacional de Estadística e Informática-INEI. Perú: Enfermedades transmisibles y no transmisibles, 2019. Lima: INEI, 2020. Disponible en: https://proyectos.inei.gob.pe/endes/2020/SALUD/ENFERMEDADES_ENDES_2020.pdf [ Links ]
4. Paoli A. Ketogenic diet for obesity: friendo or foe?. Int J Environ Res Public Health. 2014;11(2):2092-107. DOI: 10.3390/ijerph110202092. [ Links ]
5. Kahleova H, Lloren J, Mashchak A, Hill M, Fraser G. Meal frequency and timing are associated with changes in body mass index in adventist health study 2. J Nutr. 2017;147:1722-8. DOI: 10.3945/jn.116.244749. [ Links ]
6. Ha K, Song Y. Associations of Meal Timing and Frequency with Obesity and Metabolic Syndrome among Korean Adults. Nutrients. 2019;11(10). DOI: 10.3390/nu11102437. [ Links ]
7. Xiao Q, Garaulet M, Scheer F. Meal timing and obesity; interactions with macronutrient intake and chronotype. Int J Obes. 2019;43(9):1701-1711. DOI: 10.1038/s41366-018-0284-x. [ Links ]
8. Mattson M, Allison D, Fontana L, Harvie M, Longo V, Malaisse W, et al. Meal frequency and timing in health and disease. PNAS. 2014;11(47):16647-16653. DOI: 10.1073/pnas.1413965111. [ Links ]
9. Hutchison A, Heibronn L. Metabolic impacts of altering meal frequency and timing-Does when we eat matter?. Biochimie. 2016;124:187-197. DOI: 10.1016/j.biochi.2015.07.025. [ Links ]
10. Chamorro R, Farias R, Periano P. Regulación circadiana, patrón horario de alimentación y sueño: Enfoque en el problema de obesidad. Rev chil nutr. 2018;45(3). DOI: http://dx.doi.org/10.4067/s0717-75182018000400285 [ Links ]
11. Calvo J, Gianzo M. Los relojes biológicos de la alimentación. Nutr Hosp. 2018;35(4). DOI: https://dx.doi.org/10.20960/nh.2122 [ Links ]
12. Barrington W, Beresford S. Eating Occasions, Obesity and Related Behaviors in Working Adults: Does it Matter When You Snack?. Nutrients. 2019;11(10):2320. DOI: 10.3390/nu11102320. [ Links ]
13. Yoshida J, Eguchi E, Nagaoka K, Ito T, Ogino K. Association of night eating habits with metabolic syndrome and its components: a longitudinal study. BMC Public Health. 2018; 18: 1366. DOI: 10.1186/s12889-018-6262-3. [ Links ]
14. Kutsuma A, Nakajima K, Suwa K. Potential Association between Breakfast Skipping and Concomitant Late-Night-Dinner Eating with Metabolic Syndrome and Proteinuria in the Japanese Population. Scientifica (Cairo) 2014;2014:253581. DOI: 10.1155/2014/253581. [ Links ]
15. Berg C, Lappas G, Wolk A, Strandhagen E, Toren K, Rosengren A, et al. Eating patterns and portion size associated with obesity in a Swedish population. Appetite. 2009;52:21-26. DOI: 10.1016/j.appet.2008.07.008. [ Links ]
16. Guinter M, Park Y, Steck S, Sandler D. Day-to-day regularity in breakfast consumption is associated with weight status in a prospective cohort of women. Int J Obes (Lond). 2020;44(1):186-194. DOI: 10.1038/s41366-019-0356-6. [ Links ]
17. Odegaard A, Jacobs D, Steffen L, Van Horn L, Ludwig D, Pereira M. Breakfast frequency and development of metabolic risk. Diabetes Care. 2013;36(10):3100-6. DOI: 10.2337/dc13-0316. [ Links ]
18. Goto M, Kiyohara K, Kawamura T. Lifestyle risk factors for overweight in Japanese male college students. Public Health Nutr. 2010;13(10):1575-80. DOI: 10.1017/S1368980009992813. [ Links ]
19. Holmbäck I, Ericson U, Gullberg B, Wirfält E. A high eating frequency is associated with an overall healthy lifestyle in middle-aged men and women and reduced likelihood of general and central obesity in men. Br J Nutr. 2010;104:1065-1073. DOI: 10.1017/S0007114510001753. [ Links ]
20. Aljuraiban G, Chan Q, Oude L, Brown J, Daviglus M, Stamler J, et al. The impact of eating frequency and time of intake on nutrient quality and Body Mass Index: the INTERMAP Study, a Population-Based Study. J Acad Nutr Diet. 2015;115,4:528-36.e1. DOI: 10.1016/j.jand.2014.11.017. [ Links ]
21. Van der Heijden A, Hu F, Rimm E, Van Dam R. A prospective study of breakfast consumption and weight gain among U.S. men. Obesity (Silver Spring). 2007;15(10):2463-9. DOI: 10.1038/oby.2007.292. [ Links ]
22. Canuto R, Pattussi M, Macagnan J, Henn R, Olinto M. Sleep deprivation and obesity in shift workers in southern Brazil. Public Health Nutr. 2014; 17(11): 2619-23. DOI: 10.1017/S1368980013002838. [ Links ]
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: March 02, 2022; Accepted: June 20, 2022











 texto en
texto en