Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.3 Lima jul./set. 2022 Epub 09-Jul-2022
http://dx.doi.org/10.25176/rfmh.v22i3.3242
Clinical Case
Mucinous adenocarcinoma of the cecal appendix
1María Auxiliadora General Hospital. Lima Peru
Introduction:
Adenocarcinoma of the cecal appendix occurs in approximately 0.1 to 0.2% of all appendectomies. One subtype, mucinous adenocarcinoma, represents 0.08% of all neoplasms. Diagnosis is usually incidental and surgery is the best treatment option.
Clinical Case:
We describe the case of a 55-year-old male patient, evaluated for severe pain in the right iliac fossa, who was found to have an appendiceal mass during an open appendectomy. A fragmented appendix measuring 7 x 1.8 x 0.8cm, with mucoid content in its lumen; as well as mucin pools in more than 50% of the sample and signet ring cells in light microscopy revealed the pathological diagnosis of mucinous adenocarcinoma. Therefore, the pathological analysis of surgical pieces is transcendental, since there are infrequent diagnoses that can change the prognosis and course of clinical management of a patient.
Keywords: Appendectomy; Adenocarcinoma; Appendix. (fuente: MeSH NLM).
INTRODUCTION
Cecal appendix tumors are classified as serrated lesions and polyps, mucinous neoplasms, adenocarcinomas, and neuroendocrine neoplasms (NENs)1. The most frequent neoplasms of the cecal appendix are neuroendocrine tumors, which represent 85% of all tumors in this organ2. Appendicular adenocarcinoma is a rarity within appendicular neoplastic pathology and is defined as a malignant glandular neoplasm characterized by invasion1. This entity is diagnosed incidentally in approximately 0.1 to 0.2% of all appendectomies performed, corresponding to an estimated incidence of 0.2 per 100,000 patients per year1.
Unlike neuroendocrine tumors that are located in the submucosal and/or muscular layer, appendiceal adenocarcinoma originates in the mucosa and presents a more complex and irregular infiltrative pattern2. Within adenocarcinomas, there are three histological subtypes: mucinous, non-mucinous, and signet ring cell (more than 50% of the tumor are signet ring cells)1. Appendicular adenocarcinomas are designated as mucinous if more than 50% of the lesion contains extracellular mucin1,3. Mucinous adenocarcinoma of the appendix is a rare neoplasm with an incidence rate of 0.08% of all neoplasms and constitutes approximately 50% of appendiceal adenocarcinomas and only 10% of colonic adenocarcinomas1,3.
The presentation of this clinical case of mucinous adenocarcinoma of the cecal appendix was decided, due to the infrequency of incidentally finding this entity in an appendectomy due to acute appendicitis.
DESCRIPTIONOFTHECLINICAL CASE
The case of a 55-year-old male patient is presented with no significant medical and/or surgical history. The patient was admitted as an emergency with very intense colicky pain in the right iliac fossa and was evaluated under general surgery. Following his evaluation, the general surgeon decides to perform an emergency open appendectomy. The operative findings revealed an appendicular mass made up of the omentum, cecum, and thin loop, with purulent content of approximately 60 ml; and a cecal appendix digested in the distal third, with a necrotic base, to rule out an appendiceal abscess.
After the completion of the operative act, the surgical specimen, soaked in formalin, was sent to the Pathological Anatomy Service. In the Pathological Anatomy service, a fragmented cecal appendix of approximately 7 x 1.8 x 0.8cm was received, with light brown serosa, approximately 30% covered by fibrin, and with a mucoid content in the appendicular lumen. .
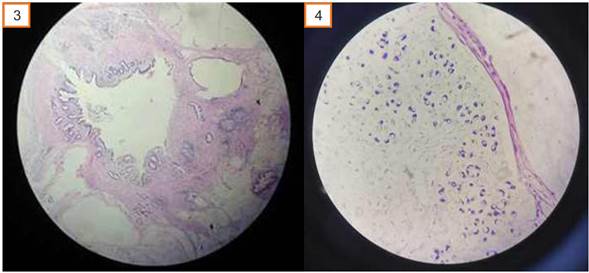
Optical microscopy revealed mucin pools or lakes in more than 50% of the sample (Figures 1y 2), with extensive invasion, infiltrating the muscular and subserosal layers. Likewise, some signet ring cells were also observed (Figures 3 y 4). At higher magnification, foci of high-grade cellular dysplasia and atypical mitoses were also observed. Surgical margins could not be evaluated due to the fragmentation of the sample. Fulfilling the histopathological criteria, the diagnosis of mucinous adenocarcinoma was established.
After the anatomopathological study, a clinical-pathological correlation was suggested to rule out primary tumor versus metastatic tumor. The only treatment that was given to the patient was surgery, with a probability of a surgical reintervention, according to subsequent imaging studies.
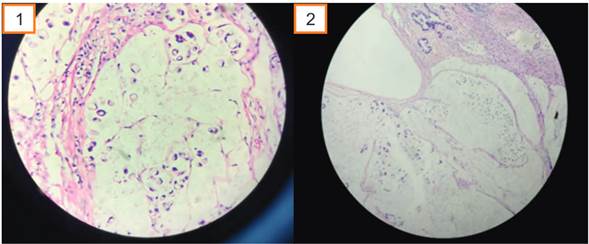
Figure 1y 2: Mucin pools in more than 50% of the sample, showing the invasive pattern of the tumor with stromal desmoplasia, an important characteristic of mucinous adenocarcinoma (HE 10x).
DISCUSSION
Adenocarcinoma of the cecal appendix is a rare entity, and the mucinous adenocarcinoma subtype is much rarer2. Appendicular adenocarcinoma is defined as a malignant glandular neoplasm characterized by invasion1. This entity is diagnosed incidentally in approximately 0.1 to 0.2% of all appendectomies performed, corresponding to an estimated incidence of 0.2 per 100,000 patients per year1.
Among the mucinous appendicular neoplasms, we find low-grade appendicular mucinous neoplasm (LAMN), high-grade appendicular mucinous neoplasm (HAMN), and also mucinous adenocarcinoma1. These mucinous neoplasms are graded according to a three-grade system. LAMN is grade 1 tumors. HAMN and mucinous adenocarcinoma are grade 2 tumors. And tumors with unequivocal signet ring cells are grade 3, all of which are specified in detail in Table 1 1. .
LAMN is a term recommended for lesions formerly classified as mucinous tumors of uncertain malignant potential, mucinous cystadenocarcinoma, or mucinous cystadenoma1. The mucin in LAMN can dissect through the structures of the cecal appendix, and extend to the peritoneal surface or cause rupture of the appendix, which is called pseudomyxoma peritoneal1. Peritoneal pseudomyxoma is a clinical entity defined in other reviews as a disease characterized by the presence of a free mucinous substance in the abdominal cavity, associated with a primary mucinous tumor and implants of mucin-producing columnar epithelium in the peritoneum and omentum(2). When pseudomyxoma peritoneal (or also called mucinous peritoneal carcinoma, which occurs when the growth of mucinous neoplastic cells causes gelatinous ascites in the peritoneal cavity) is present, the distinction between low-grade and high-grade has prognostic significance; likewise, if the mucin deposited is acellular, the prognosis is better2. The most frequent origin of peritoneal pseudomyxoma is mucinous tumors of the appendix and ovary2, which is why the presence of these other tumors is always inquired about, mainly in female patients.
Appendicular adenocarcinoma has a predominance in males and the age between 50 and 70 years, as evidenced in different series and reviews4-6. In the present report, the predominance of the male sex in this entity is verified, as well as the greater frequency close to the sixth decade of life; results reported in a similar way by other authors2,4,5,7.
In most cases, patients with appendiceal adenocarcinoma present with a clinical picture of acute appendicitis, and the diagnosis is generally made during or after surgery2,6. Other patients present with obstruction, palpable mass, or intestinal bleeding. If this neoplasm spreads throughout the peritoneal cavity, producing pseudomyxoma peritonei, it can form large amounts of mucus, which can cause abdominal distention and even accumulation of mucus within a hernial sac. In the case of the patient in this clinical case, intense pain was observed in the right iliac fossa, which simulated acute appendicitis.
The causes of an appendiceal adenocarcinoma are not clear, but it has been associated with other neoplasms in the small intestine, chronic ulcerative colitis, and with appendiceal adenoma1,2.
In the surgical piece that arrived at the pathological anatomy department, which consisted of a fragmented appendiceal sample, mucin pools or lakes were found in more than 50% of the tumor, which infiltrated until reaching the muscular and subserosal layers. Likewise, some signet ring cells were observed floating in the mucin pools. Taking into account the histopathological criteria described in Table 1, the final diagnosis of mucinous adenocarcinoma was made, ruling out important differential diagnoses such as appendiceal adenoma, an entity in which there is no invasion, and the muscularis mucosae remains intact2.
Dissemination to the peritoneal cavity occurs in both high-grade appendiceal mucinous neoplasia (HAMN) and mucinous adenocarcinoma, and should not be the only factor in distinguishing these two entities1. There are clear criteria to distinguish low and high grade mucinous neoplasms from mucinous and signet ring cell adenocarcinomas, which are detailed inTable 1 1.
It is important to mention that the presence of a signet ring cell pattern in an adenocarcinoma also requires ruling out a metastatic origin2. In some literature, it is also specified that when there is the presence of signet ring cells in an appendiceal tumor of probably primary origin, it is necessary to make a differential diagnosis with a metastasis of a primary gastric lesion (an almost impossible task in the absence of necropsy)6.
Table 1. Histological criteria for grading appendiceal mucinous neoplasms, and adenocarcinomas and their peritoneal metastases(1)
| TUMOR GRADE HISTOLOGICAL | CRITERIA | ||
| In primary appendiceal tumor | In peritoneal metastasis | ||
| 1 | LAMN (Low-grade appendiceal mucinous neoplasm): Low-grade cytology (atypia mild, columnar cells with nuclear pseudostratification), with a pushing margin (“Pushing margin”), that is, the tumor covers a jagged and fibrotic appendiceal wall, without infiltrative-type invasion. | ▪ Hypocellular mucinous deposits ▪ Neoplastic epithelial elements with low-grade cytology. ▪ No infiltrative type invasion. | |
| 2 | ▪ HAMN (High-grade appendiceal mucinous neoplasm): High-grade cytology (enlargement, hyperchromasia and nuclear pleomorphism, atypical mitoses and cellular necrosis), with a pushing margin ("Pushing margin"), that is, the tumor covers a wall toothed and fibrotic appendiceal, without infiltrative-type invasion. ▪ Invasive mucinous adenocarcinoma (more than 50% tumor with extracellular mucin), without signet ring cell component. (The presence of signet ring cells in the peritoneal mucin has prognostic significance even if they do not constitute more than 50% of the tumor) [Signet ring cells must be distinguished from degenerated tumor cells in the mucin (pseudo-signet ring cells). )]. | ▪ Hypercellular mucinous deposits, seen at 20X ▪ High-grade cytological features. ▪ Infiltrative-like invasion characterized by angulated or toothed glands, in a desmoplastic stroma, or with a small mucin cluster pattern with numerous mucin clusters containing clusters of tumor cells. | |
| 3 | Signet-ring cell adenocarcinoma, with numerous signet-ring cells (more than 50% of the tumor) in pools of mucin, or infiltrating appendicular tissue (signet-ring cells must be unequivocal). | Mucinous tumor deposits with signet ring cells. | |
In the case of mucinous neoplasms involving the peritoneum, the American Joint Committee on Cancer (AJCC) recommends a 3-level classification scheme, since the prognostic importance of three groups has been demonstrated in multiple studies for this type of tumor3. The 3-tier scoring scheme proposed by the AJCC is based on cytologic features, tumor cellularity, and the presence of a signet ring component (Table 2)3. In case of doubt to grade, the highest grade should be assigned to the staging3,7
Table 2. Grading of mucinous neoplasms involving the peritoneum(3)
| Well differentiated (G1) | Low-grade cytological atypia, without ring cells stamp. Tumors involving the peritoneum show acellular mucin or low cellularity (usually less than 20%), and lack invasion of the peritoneal and/or other organs. |
| Moderately differentiated (G2) | Mixture of high-grade and low-grade cytologic atypia, or diffuse high-grade cytologic atypia, not signet-ring cells. |
| Probably differentiated (G3) | High-grade cytological atypia, usually with a signet ring cellular component. |
Appendicular mucinous adenocarcinoma has only been described in a few hundred cases (incidence of 0.12 to 0.95 per million people) and due to its low incidence, there is no single optimal treatment; however, the treatment of choice is surgery8, which was performed on the patient in this case report.
However, from the oncological point of view, given the lymphatic spread of these tumors, right hemicolectomy is the surgical treatment of choice2,9. This treatment is also the most appropriate when the neuroendocrine neoplasms are larger than 2 cm, compromise the base of the tumor, and when there is the presence of villous adenomas due to the risk of malignancy and the possibility of recurrence2.
Regarding the prognosis of appendiceal adenocarcinomas, the characteristics that have been associated with a worse prognosis are advanced age, high histological grade and non-mucinous histology2. Mucinous adenocarcinomas with a lesser degree of differentiation (G2 and G3) can also produce peritoneal pseudomyxoma, but they more frequently invade the underlying organs and exhibit hematogenous and lymphatic metastases1.
Appendectomy is reserved for cases of adenocarcinoma in which the tumor is well localized and differentiated2. Laparoscopic tumor resection can be related to peritoneal dissemination, so it should be avoided2. The use of 5-fluorouracil has also been described, after surgery, with a treatment of six cycles, with which a 75% survival rate has been obtained2.
CONCLUSIONS
This clinical case is about a mucinous adenocarcinoma of the cecal appendix, which presents as an appendicular mass, ruling out an abscessed infectious process, originating from acute appendicitis.
The vast majority of cecal appendages that reach the pathological anatomy services correspond to an inflammatory process, that is, to an acute appendicitis, or alternatively, to an appendiceal abscess. With this case report, we seek to raise awareness and highlight the importance that every surgical piece resulting from an appendectomy be evaluated meticulously and in detail, since, as in this case, sometimes we can come across infrequent diagnoses that can change the prognosis and course of clinical management of said patient. An early diagnosis will allow the patient to receive optimal surgical treatment as soon as possible.
REFERENCES
1. World Health Organization. Classification of tumours: Digestive System Tumours. 5 edition. 2019; 1. Disponible en: https://publications.iarc.fr/Book-And-Report-Series/Who-Classification-Of-Tumours/Digestive-System-Tumours-2019 [ Links ]
2. Iñaguazo D., Mora J., Carrillo L. Neoplasias del apéndice: Reporte de un caso de adenocarcinoma. Gaceta Mexicana de Oncología. 2007; 6 (1). Disponible en: https://www.imbiomed.com.mx/articulo.php?id=45938 [ Links ]
3. Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin. 2017;67(2):93-9. https://doi.org/10.3322/caac.21388 [ Links ]
4. Nitecki SS, Wolff BG, Schlinkert R, Sarr MG. The natural history of surgically treated primary adenocarcinoma of the appendix. Ann Surg. 1994;219(1):51-7. https://doi.org/10.1097/00000658-199401000-00009 [ Links ]
5. Galano Urgellés R, Casaus Prieto A, Rodríguez Fernández Z. Adenocarcinoma primario del apéndice cecal. Rev Cuba Cir. 1998; 37(2):119-25. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_abstract&pid=S0034-74931998000200008&lng=es&nrm=iso&tlng=es [ Links ]
6. Ito H, Osteen RT, Bleday R, Zinner MJ, Ashley SW, Whang EE. Appendiceal adenocarcinoma: long-term outcomes after surgical therapy. Dis Colon Rectum. 2004;47(4):474-80. https://doi.org/10.1007/s10350-003-0077-79 [ Links ]
7. Burgart L, Shi C, Driman D, Fitzgibbons P, Frankel W, Hill K, et al. Protocol for the Examination of Specimens From Patients With Carcinoma of the Appendix. College of American Pathologists. 2020. Disponible en: https://www.cap.org/protocols-and-guidelines/cancer-reporting-tools/cancer-protocol-templates [ Links ]
8. Wolniczak I, Cáceres del Águila A, Santillana Callirgos JA. Adenocarcinoma mucinoso de apéndice: Reporte de un caso. Rev Gastroenterol Perú. 2016;36(2):169-71. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_abstract&pid=S1022-51292016000200011&lng=es&nrm=iso&tlng=es [ Links ]
9. Venturelli M F, Cáceres P M, Meza A R, Cárcamo I M, Garcés Q B, Miranda U M. Tumores apendiculares en 6.093 apendicectomías de urgencias: Sobrevida a 5 años. Rev Chil Cir. 2010;62(6):594-9. Disponible en: http://www.scielo.cl/scielo.php?script=sci_abstract&pid=S0718-40262010000600009&lng=es&nrm=iso&tlng=es [ Links ]
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: September 02, 2021; Accepted: May 20, 2022











 texto en
texto en