Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.3 Lima jul./set. 2022 Epub 09-Jul-2022
http://dx.doi.org/10.25176/rfmh.v22i3.4984
Letters
Impact of the Covid-19 pandemic in a specialized tuberculosis unit
1Universidad Ricardo Palma, Lima, Peru.
2Instituto de Investigación de Ciencias Biomédicas, Lima, Peru.
Dear editor,
The COVID-19 pandemic has negatively affected other disease prevention and control programs that could cause more deaths than the coronavirus itself1, and also having substantial consequences for other domains, such as social impact: slowing economic growth and increasing rates of unemployment, poverty, and food insecurity.
The pandemic context generated a particular concern for the regular provision of health services since human and infrastructure resources for medical care were transferred to services related to COVID-19, for this reason, patients with health problems health not related to COVID-19 were abandoned by not having access to health care services2. Consequently, control measures and epidemiological surveillance of tuberculosis (TB) were affected, which would produce an increase in the number of cases3.
Peru is one of the countries with the highest incidence of tuberculosis, both sensitive and resistant, in the world. Although the public health measures adopted in the country have improved the care, diagnosis and management of People Affected by TB (PAT), there are still limitations in the control of the disease, especially in multidrug-resistant TB (MDR), People Deprived of Freedom (PDF) and People Living with HIV (PLWHIV), as referred to by Guin et al.4.
According to data from the World Bank, between 40 and 60 million people will have fallen into extreme poverty in 2020 as a result of COVID-19, knowing the close relationship between poverty and TB, an increase in prevalence and incidence is expected to medium and long term1.
Both COVID-19 and TB affect the respiratory system, primarily the lungs, and have similar symptoms such as cough, fever, and shortness of breath, although the severity and duration of symptoms vary1. But, COVID-19 has overtaken TB as the infectious disease with the highest death rate per day5. Comorbidities such as chronic kidney disease, diabetes, lung cancer, and chronic obstructive pulmonary disease (COPD), especially secondary to smoking, have a higher risk of hospitalization and death when related to COVID-19 and/or TB6. A preventive measure to prevent the spread of SARS-CoV-2 was mandatory social isolation at home, however, this measure could facilitate the transmission of TB, due to prolonged contact at home7.
During the COVID-19 pandemic (2020-2021), in the Specialized Tuberculosis Unit of the Pulmonology Service at Hospital Nacional Dos de Mayo, a more than double increase in the prevalence of hospitalized patients with Type 2 Diabetes Mellitus (DM2) and TB (Figure 1) ompared to the periods prior to the pandemic (2015-2019); which could be explained as a secondary effect of poor control of the disease, late diagnosis and inadequate follow-up of chronic diseases, due to the insufficient functioning of the first level of care8.
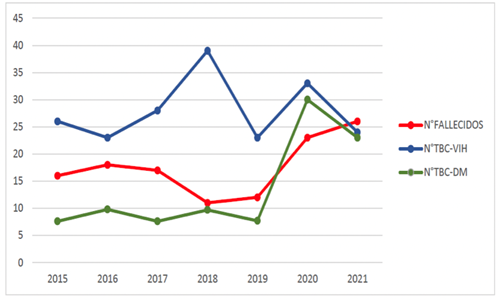
Figure 1. Annual frequency of cases hospitalized for tuberculosis and type 2 diabetes mellitus (green line), tuberculosis and HIV (blue line), and deaths from tuberculosis (red line)
The average uptake of respiratory symptoms decreased by 46.8% during the pandemic period, compared to the pre-pandemic period (Figure 2); however, no change was found in the percentage of positive smear microscopy when we compared the period prior to the pandemic (3.7%) with the period of the pandemic (3.8%). In addition, we evidenced that there was no change in the average number of hospitalizations of patients with MDR-TB9.
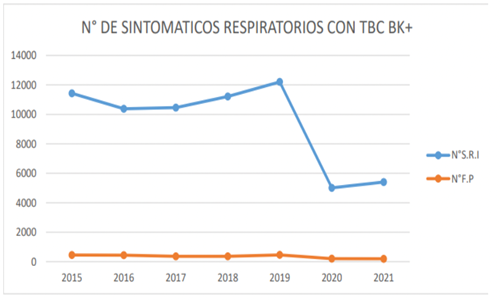
Figure 2. Annual frequency of detection of respiratory symptoms (blue line) and annual frequency of positive smears for M. tuberculosis (orange line)
Finally, the average number of deaths hospitalized for tuberculosis increased by 60% during the pandemic (Figure 1), compared to the previous period; this would be due to the late diagnosis of the disease and hospitalization due to severe complications, such as meningoencephalitis (MEC), TB and TB with respiratory failure10.
Today, two years after the pandemic began in Peru, the ambitious challenge is to mitigate its effects, without neglecting pre-existing diseases, especially remembering that both infections share social determinants of health, related to poverty, which today would have increased after confinement throughout Peru.
In addition, any investment made in the management of the coronavirus should be used for the care of TB patients; citing as examples effective social isolation, hand washing, and mandatory use of a mask in closed public places. Similarly, the implementation of new molecular laboratories to optimize and speed up the diagnosis of TB in the future. The current situation is radically changing the way we manage TB for the foreseeable future and unmasking vulnerabilities; it is necessary to get back on track, in order to avoid an unprecedented health crisis11.
REFERENCES
1. Santin M. La pandemia de COVID-19 amenaza la lucha contra la tuberculosis. The Conversation [Internet]. 2021. Disponible en: https://theconversation.com/la-pandemia-de-covid-19-amenaza-la-lucha-contra-la-tuberculosis-149756 . [ Links ]
2. Fuady A, Houweling TAJ, Richardus JH. Costos catastróficos relacionados con COVID-19 y tuberculosis. Am J Trop Med Hyg. 2020; 104 (2): 436-440. [ Links ]
3. Khan F, Kazmi Z, Hasan M, Dos Santos Costa A, Ahmad S, Essar M. Resurgimiento de tuberculosis en medio de COVID-19 en Perú: Factores de riesgo asociados y recomendaciones. Gerente de Plan de Salud Int J. 2021; 36 (6): 2441-2445. [ Links ]
4. Guinn, K. M., & Rubin, E. J. Tuberculosis: Just the FAQs.MBio. 2017; 8(6), e01910-17. https://doi.org/10.1128/mBio.01910-17 [ Links ]
5. Hogan, A. B., Jewell, B. L., Sherrard-Smith, E., Vesga, J. F., Watson, O. J., Whittaker, C., et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. The Lancet. Global health. 2020; 8(9), e1132-e1141. https://doi.org/10.1016/S2214-109X(20)30288-6 [ Links ]
6. Visca, D., Ong, C., Tiberi, S., Centis, R., D'Ambrosio, L., Chen, B., Mueller, J., Mueller, P., Duarte, R., Dalcolmo, M, Sotgiu, G., Migliori, GB y Goletti, D. Interacción entre tuberculosis y COVID-19: una revisión de los efectos biológicos, clínicos y de salud pública. Neumología. 2021; 27(2),151-165. https://doi.org/10.1016/j.pulmoe.2020.12.012 [ Links ]
7. Madrid R, Jorquera P, Jaramillo Y. Impacto de la pandemia Covid -19 sobre el programa de tuberculosis infantil. Rev Neumología Pediátrica. 2022; 17 (1): 26-27. [ Links ]
8. Hogan A, Jewell B, Sherrard-Smith E, Vesga J, Watson O, Whittaker C, et.al.Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020; 8 (9). https://doi.org/10.1016/S2214-109X(20)30288-6 [ Links ]
9. Fuady A, Houweling T, Richardus J. Costos catastróficos relacionados con COVID-19 y tuberculosis. Am J Trop Med Hyg. 2020; 104 (2): 436-440. [ Links ]
10. Desaliñado DW. ¿La pandemia de COVID-19 ha aumentado la mortalidad por tuberculosis? La lanceta. Enfermedades infecciosas. 2022; 22 (2), 165-166. https://doi.org/10.1016/S1473-3099(22)00006-8 [ Links ]
11. Aguilar P, Cotrina J, Zavala E. Infeccion por SARS-CoV-2 y tuberculosis pulmonar: análisis de la situación en el Perú. Cadernos de Saúde Pública [Internet]. 2020; 36(11). Disponible en: https://doi.org/10.1590/0102-311X00094520 [ Links ]











 texto en
texto en 


