Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.4 Lima oct./dic. 2022 Epub 12-Oct-2022
http://dx.doi.org/10.25176/rfmh.v22i4.5045
Original article
Post-infection sequelae of COVID 19 among patients of Hospital I Florencia de Mora. Trujillo - Peru
1Universidad César Vallejo - Facultad de Medicina Humana
Introduction:
COVID-19 is a disease with predominance of respiratory and other organ and system symptoms and unlike other viruses, it may present sequelae. The terms post-acute COVID and chronic COVID have been suggested for patients with symptoms or signs of illness of three weeks and three months, respectively, after the onset of acute COVID-19. In this context, interest arose in establishing a baseline and follow-up to identify sequelae in patients diagnosed with COVID-19.
Objectives:
To identify post COVID-19 sequelae in patients with medical discharge for this pathology.
Methods:
A prospective descriptive study was conducted between the second and fourth quarter of 2021 with a population of 330 patients diagnosed with COVID-19. Baseline was established at the beginning of the study, followed by follow-up and control consultation to identify post-COVID-19 sequelae and to perform control spirometry.
Results:
The frequency of COVID-19 was 29.78% (330 cases/1108 attended). 43.94% of positive cases were in the 40-59 years age group, 28.8% (95/330) referred as comorbidity: cardiovascular disease, diabetes mellitus II and bronchial asthma. Post COVID-19 sequelae predominated: respiratory (61%), musculoskeletal (43%) and neurological (20%), with dyspnea, dorsalgia and headache, respectively. The duration of sequelae ranged from 21 days to seven months, spirometry showed a mild restrictive pattern in patients aged 41 to 50 years, all female.
INTRODUCTION
COVID-19 is an infection caused by SARS-CoV2 that was characterized as a pathological entity with an unknown natural history before the onset of cases was reported worldwide. Aspects related to the mechanism of transmission, risk factors, clinical picture, complications, sequelae, and treatment became progressively known.
As for the clinical picture, the following symptoms have been described: fever, cough, muscle aches or fatigue, respiratory distress of varying intensity, (1,2-5) odynophagia, liquid stools, nausea,(1,2,4,6), abdominal pain,(3-5), dizziness, headache, alteration of the senses (taste and smell),(2,4)joint pain,(3)disorders of consciousness, rashes on the skin such as wheals, blisters or purpura.(2)This wide variety of symptoms disappears 10 - 15 days after the onset of the clinical picture; however, the contagiousness and spread of the virus persist.(1)
Unlike other viral infections, COVID-19 has been described with different sequelae that affect the quality of life, with predominance of the respiratory system (dyspnea, fatigue, pulmonary fibrosis),(7-9)cardiovascular (increased resting heart rate, myocarditis, arterial hypertension),(10,11)neurological (headache, anosmia, ageusia),(12-14)psychological (with predominance of depression and anxiety), renal (with the possibility of renal failure) and osteomuscular (arthralgias, myalgias);(15-17)among others.
Peru is one of the countries most affected worldwide by COVID-19 infection, with high mortality rates and probably a large number of sequelae to be documented. The La Libertad region had a large number of cases and deaths from this disease in all its districts, with a predominance of Trujillo and La Esperanza, with 90,122 cases and 10,226 deaths documented in the entire region as of November 2021.(18) This large number of patients is usually followed up to see their evolution, but the types and frequency of sequelae following COVID-19 infection have not been documented. In many cases, the facilities have a database with all the information on these patients on admission, during hospitalization or at discharge but do not have information on the sequelae; hence the interest arose to study the evolution of the cases presented in the Florencia de Mora District attended at the Hospital I of EsSALUD, where in August 2020, COVID-19 prevalence of 74.90% was reported in a population of 2,622 screened patients.(19)
This research presents the findings of patients attended at the Hospital I Florencia de Mora - ESSALUD with the following study objectives: to identify post-COVID-19 sequelae in patients attended between the second and fourth quarter of 2021 and specific objectives: to formulate the baseline of COVID-19 infection, to follow up during the third and fourth quarter of 2021 of people with positive diagnostic tests for COVID-19 and to identify the type and frequency of post-COVID-19 sequelae.
METHODS
Design and study area
A prospective longitudinal study was conducted based on a review of the medical records and epidemiological files of patients with COVID-19 registered at the EsSALUD Hospital in Florencia de Mora (HIFM) corresponding to the second quarter of 2021.
Population and sample
Using non-probabilistic convenience sampling, the population consisted of 1280 patients seen in differentiated triage at the HIFM during the second quarter of 2021.
Inclusion and exclusion criteria
Patients were included if they met the following criteria: they were of both sexes, from the hospital's jurisdiction and agreed to participate in the study. From this group, patients who showed sequelae during the control interview and who had positive laboratory results for the detection of the causal agent of COVID-19 were selected, with prior informed consent. Patients with persistent dyspnea or chronic cough underwent pulmonary function evaluation by spirometry. Patients with pre-existing chronic respiratory or neurological pathology, rheumatoid arthritis or under immunosuppressive treatment were excluded from the study.
Variables, instruments and procedures
Each of the activities proposed in this longitudinal study was developed: baseline and follow-up medical examination. The baseline of the COVID-19 cases of this facility was elaborated, as well as the analysis of the follow-up consultation report to update the anamnesis and identify possible sequelae in these patients. The information collected was subjected to processing in Excel and SPSS for descriptive statistical analysis.
Ethical aspects
Authorization was obtained from the Management of the Hospital I Florencia de Mora to carry out this research and the ethical principles of beneficence, non-maleficence, autonomy and justice were taken into account, as well as biosafety measures through the use of primary protection equipment. Informed consent was given and the confidentiality and veracity of the data collected was maintained. This project was approved by the Ethics Committee of the School of Medicine - Universidad César Vallejo (Report 003-CE-FCS-UCV-21) and is registered in the National Health Research Registry (PRISA) with code: EI00001980.
RESULTS
A total of 1280 epidemiological records of patients attended in the COVID Triage of the Hospital I Florencia de Mora during the second quarter of 2021 were evaluated, of which only 1108 patients showed diagnosis of COVID-19 infection with different tests and 172 patients with COVID-19 diagnosis based on the clinical picture present, which motivated their exclusion from the study.
300 patients of both sexes were diagnosed positive for COVID-19 (29.78%) with individual or combined diagnostic tests. The antigenic test was applied in 96.39% and the molecular test in only 1.81% of the population studied.
Table 1. Diagnosis of COVID-19 according to age group and sex in patients seen at Hospital I Florencia de Mora, second quarter 2021.
| Age | SEX | Total | |||||||
| Female | Male | ||||||||
| N° | % | N° | % | N° | % | ||||
| <= 5 years | 100,0 | 0 | 0,0 | 0,91 | |||||
| 6 - 9 years | 60,0 | 40,0 | 5 | 1,52 | |||||
| 10 - 19 years | 42,9 | 57,1 | 6,36 | ||||||
| 20 - 29 years old | 38,6 | 61,4 | 13,33 | ||||||
| 30 - 39 years old | 43,9 | 56,1 | 20,00 | ||||||
| 40 - 59 years | 46,2 | 53,8 | 145 | 43,94 | |||||
| 60 - 79 years | 58,1 | 41,9 | 43 | 13,03 | |||||
| >= 80 years | 100,0 | 0 | 0,0 | 0,91 | |||||
| Total | 47,3 | 174 | 52,7 | 330 | |||||
The age group 40-59 years showed 43.94% of positive results for SARS-CoV-2. Likewise, 100% of women younger than 5 years and older than 80 years had positive diagnostic tests.
Table 2. Distribution of the population with diagnosis of COVID-19 according to comorbidity and sex. Hospital I Florencia de Mora, second quarter 2021.
| COMORBILITY | SEX | TOTAL | ||||
|---|---|---|---|---|---|---|
| MALES | WOMEN | |||||
| N | % | N | % | N | % | |
| Cardiovascular disease | 35,94 | 64,06 | 64,65 | |||
| Diabetes Mellitus II | 57,14 | 42,86 | 14,14 | |||
| Bronchial asthma | 5 | 41,67 | 58,33 | 12,12 | ||
| Gestation | 0 | 0 | 4,04 | |||
| Cancer | 0 | 0 | 5 | 5 | 5,05 | |
| Total | 36,36 | 63,64 | 99 | 100% | ||
Thirty percent (99 of 330) of the COVID-19 patients showed comorbidity; cardiovascular disease was the most frequent comorbidity (64.65%), predominantly in women, followed by diabetes mellitus (14.14%), which predominated among men, and bronchial asthma (12.12%), which predominated in women.
Regarding the follow-up performed between October and December 2021 on the 330 patients with COVID-19 to evaluate their clinical evolution and identify the presence of post-discharge sequelae, the following results are presented:
Table 3. Presence of sequelae in the population diagnosed with COVID-19. Florencia de Mora Hospital I, December 2021.
| N° | % | ||||
| Sequels | Yes | 95 | 28,8 | ||
| No | 51,8 | ||||
| Not located | 19,4 | ||||
| Total | 330 | 100,0 | |||
Table 4. Population with positive COVID-19 diagnosis according to time of presentation and type of sequelae. Florencia de Mora Hospital I, December 2021.
| Presentation time in days | N | % | ||
|---|---|---|---|---|
| 21 - 30 | 81 | 85,3 | ||
| 31 - 45 | 12,6 | |||
| 46 to more | 2,1 | |||
| Type of sequelae | N | % | ||
| Respiratory | 58 | 61,0 | ||
| Osteomuscular | 43,1 | |||
| Neurological | 20,0 | |||
| Psychological | 1 | 1,0 | ||
| Other | 8,4 | |||
| Two or more systems | - |
85.3% of patients reported the presence of sequelae between 21 to 30 days after discharge from COVID-19, 12.6% between 31 to 45 days after discharge and 2.1% reported the presence of sequelae from 46 days after discharge. The predominance of respiratory and musculoskeletal sequelae is also shown.
Table 5. Population with positive COVID-19 diagnosis according to type of sequelae and sex. Hospital I Florencia de Mora, December 2021.
| Sex | Total | ||||||
| Female | Male | ||||||
| Respiratory | Dysphagia | 33,3% | 66,7% | 100,0% | |||
| Dyspnea | 53,0% | 47,0% | 100,0% | ||||
| Dysphagia and dysphonia, Dyspnea and | 0 | 0,0% | 100,0% | 100,0% | |||
| odynophagia | 1 | 100,0% | 0 | 0,0% | 1 | 100,0% | |
| Total | 50,0% | 50,0% | 58 | 100,0% | |||
| Neurological | Headache | 50,0% | 50,0% | 100,0% | |||
| Anosmia / Ageusia | 25,0% | 75,0% | 100,0% | ||||
| Anosmia | 100,0% | 0 | 0,0% | 100,0% | |||
| Total | 47,4% | 52,6% | 100,0% | ||||
| Osteomuscular | Joint Pain | 67,0% | 1 | 33,0% | 100,0% | ||
| Muscle Pain | 0 | 0,0% | 100,0% | 100,0% | |||
| Dorsalgia | 75,8% | 24,2% | 100,0% | ||||
| Muscular hypotrophy | 1 | 50,0% | 1 | 50,0% | 100,0% | ||
| Total | 68,3% | 31,7% | 100,0% | ||||
| Psychological | Anguish, Depression | 1 | 100,0% | 1 | 100,0% | ||
| Total | 1 | 100,0% | 1 | 100,0% | |||
| Other | Hair loss | 0 | 0,0% | 100,0% | 100,0% | ||
| Digestive symptoms | 60,0% | 40,0% | 5 | 100,0% | |||
| Pruritus | 0 | 0,0% | 1 | 100,0% | 1 | 100,0% | |
| Total | 37,5% | 5 | 62,5% | 100,0% | |||
The most frequent respiratory sequela was dyspnea (84.4%) with a female predominance (53%). Among the musculoskeletal sequelae, dorsalgia predominated (77%), with the female sex being more affected. Headache was present in 42.1% of the patients with neurological sequelae, in equal proportion in both sexes. Smell and taste impairment predominated among men and psychological sequelae were reported only by men.
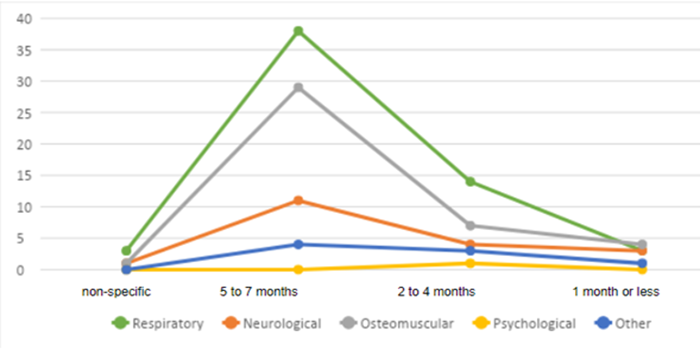
The post-COVID-19 sequelae with the longest duration are respiratory (predominantly dyspnea), followed by musculoskeletal and neurological manifestations, some of them lasting up to seven months.
Table 6. Population with positive COVID-19 diagnosis according to age, sex, risk condition, and spirometry result. Hospital I Florencia de Mora, December 2021.
| SPIROMETRY | Total | ||||||
| Normal | Mild restrictive | ||||||
| Age | 15 - 20 | 7,4% | 0 | 0,0% | 7,4% | ||
| 21 - 30 | 1 | 3,7% | 0 | 0,0% | 1 | 3,7% | |
| 31 - 40 | 14,8% | 0 | 0,0% | 14,8% | |||
| 41 - 50 | 33,3% | 7,4% | 40,7% | ||||
| 51 to more | 33,3% | 0 | 0,0% | 33,3% | |||
| Sex | F | 51,9% | 7,4% | 59,3% | |||
| M | 40,7% | 0 | 0,0% | 40,7% | |||
| Risk condition | Does not present | 63,0% | 0 | 0,0% | 63,0% | ||
| Bronchitis | 1 | 3,7% | 0 | 0,0% | 1 | 3,7% | |
| Diabetes mellitus | 1 | 3,7% | 0 | 0,0% | 1 | 3,7% | |
| Pharyngitis | 1 | 3,7% | 0 | 0,0% | 1 | 3,7% | |
| Gastritis | 1 | 3,7% | 0 | 0,0% | 1 | 3,7% | |
| Arterial hypertension | 10,8% | 0 | 0,0% | 10,8% | |||
| HTA- Diabetes | 1 | 3,7% | 0 | 0,0% | 1 | 3,7% | |
| HTA -Obesity | 0 | 0,0% | 1 | 3,7% | 1 | 3,7% | |
| Hypothyroidism | 0 | 0,0% | 1 | 3,7% | 1 | 3,7% | |
| Total | 92,3% | 7,7% | 100,0% | ||||
Interpretation: Only 7.4% of patients who manifested persistent dyspnea as a post COVID-19 sequela presented a mild restrictive pattern during spirometry. These patients belonged to the age group 41 to 50 years, female sex and had comorbidity arterial hypertension/obesity and hypothyroidism.
DISCUSSION
The prevalence of patients identified with a positive diagnosis of COVID-19 was 29.73%, much lower than that reported in the same healthcare center for the population attended in the differentiated triage during the year 2020 (74.90%).(19)In both the study by Tejada López et al,(19)and the present study, the diagnosis was mostly made with antigenic diagnostic test, compared to the molecular test applied to 1.81% of the population. Previous studies indicate that antigenic tests are less sensitive and specific than the molecular test and their titer develops as COVID-19 disease progresses in its natural history, being more sensitive in early symptomatic patients (5 to 7 days of illness).(20)
The lower number of confirmed cases of COVID-19 (330 patients) during the second quarter of 2021, compared to 2020 in the same hospital,(19)could be explained by the national trend for this disease, since the second wave of COVID-19 had already passed, which in Peru had its highest peak between March and April 2021(21)and the La Libertad region was not among the regions with the highest prevalence and attack rate for COVID-19 during that period.(22)
The predominance of males (53.03%) with evidence of COVID-19 (Table 1) has been described in different studies. The higher the prevalence of COVID-19 among males, and in terms of age, the higher the age, the higher the number of cases. In the study by Tejada et al(19), 57.5% of cases were among males, as in the study by Villagrán-Olivas K,(23)COVID-19 predominated among males in a Mexican population; however, the study by Ruiz Cantero M(24)indicates that, although initially the number of cases reported in Spain was among males, in less than a month the number of cases in females equaled that of males. It considers that these differences are due to preliminary cross-sectional measurements and to the differences in the clinical picture, with respiratory symptoms predominating in men, while dysphagia and digestive symptoms predominated in women, as well as mild clinical pictures with home or outpatient treatment. The severity of the disease was also greater in men (more hospitalizations and ICU admissions) than in women, which may have led to underreporting or to the perception that COVID-19 was more frequent in men than in women.(24)
In reference to the most affected age group, the 40-59 years age group concentrated 43.94% of cases (Table 1). in both sexes. The population aged 60 years and older presented a confirmed diagnosis of COVID 19 in 13.03%. Regarding this variable, the study by Tejada et al(19), reported 77.9% of cases in adults aged 27-59 years. Villagrán-Olivas K,(23)reported that the population aged 40 years and older was the most affected, reaching more than 50% between 40 and 65 years of age. On the other hand, Cortés et al(25)report that, in Colombia, the trends of positive cases were similar in both sexes and in terms of age, the highest number of cases occurred between 21-60 years of age. Mortality was higher in people aged 50 years and older, and the number of male deaths was higher than the number of female deaths. In the present case, no deaths were recorded during the study period.
COVID-19 is a disease characterized by a very varied clinical picture, with a predominance of respiratory symptoms and symptoms of other organs and systems, of variable intensity, (1,2-6) but that can be exacerbated when comorbidity is present. Of the 330 patients diagnosed with COVID-19, 99 reported having associated diseases (45.74% of men and 54.26% of women). Cardiovascular disease was the most frequent, being present among 64.65% of participants, followed by diabetes mellitus (14.14%) and bronchial asthma (12.12%). Both cardiovascular disease and bronchial asthma predominated among women (Table 2).
Among the national antecedents, it was found that the most frequent comorbidity was arterial hypertension,(19)in the study by Balboa CT et al(26)in the Chilean population, arterial hypertension (46%) and type 2 diabetes mellitus (27%) were the main comorbidities, which together with other pathologies such as chronic obstructive pulmonary disease, neurological pathology, prostration, and immunosuppression, increased the risk of death. In the systematic review and meta-analysis carried out by Plasencia-Urizarri et al(27)it is pointed out that chronic kidney disease, cardiovascular disease, arterial hypertension, and diabetes mellitus are among the comorbidities that can aggravate the clinical picture and the evolution of patients with COVID-19, an event (mortality) that was not observed in the population of the present study because almost all of them received outpatient care and telephone follow-up until discharge. In other studies such as that of Villagrán-Olivas K,(23)the most frequent comorbidities among patients with COVID-19 were obesity (33.3%), arterial hypertension (31.7%), and diabetes mellitus (21.9%). The author mentions that obesity is a public health problem as Mexico has a prevalence of 32.4%.
In the second phase of the study, 330 cases with positive COVID-19 were followed up. Of this group, 171 participants (51.8%) reported having fully recovered after 7 to 15 days of illness without sequelae and 95 patients (28.8%) reported having sequelae or having them at the date of the evaluation, between October and December 2021 (Table 3). In this regard, post-COVID syndrome(28)has been described, characterized by highly variable symptoms and signs that last more than three weeks after discharge.
The terms post-acute COVID have also been suggested for patients with symptoms or signs of illness lasting 3 weeks and chronic COVID when the duration is 3 months or more after the onset of acute COVID-19.(28-30)In the clinical picture of this syndrome, fatigue, shortness of breath, chest tightness, myalgia, difficulty concentrating, and sleep disturbances are frequently reported,(30)and its prevalence ranges from 20 to 90%.(28)This wide range is related to the severity of acute COVID-19.
For the purposes of this research, we have called sequelae the clinical manifestations of patients who, upon discharge after COVID-19 infection, presented symptoms or signs compatible with post-COVID syndrome,(20-22)(Table 4), finding that 28.8% of the population diagnosed with COVID-19 presented this syndrome.Table 4shows that 85.3% of the patients interviewed reported having presented sequelae between 21 and 30 days after discharge from COVID-19, 12.6% between 31 and 45 days after discharge, and 2.1% reported the presence of sequelae from 46 days after discharge, with some patients presenting symptoms up to seven months after COVID-19.
Regarding the time of presentation of sequelae, it is reported that in post hospitalized patients studied in an Italian case series, in 13% of them, symptoms lasted up to 60 days from the onset of the disease(31)and in another case series from the United Kingdom, post COVID-19 symptoms lasted between 28 and 71 days after discharge.(32)According to Carod-Artal,(33)between 10% to 65% of people with mild to moderate COVID-19 present post COVID syndrome up to 12 to more weeks after the acute picture. He also points out the great variability in the clinical presentation and duration, which could be explained by the inflammatory response in various organs, but also because there is variation in the type of populations studied (outpatient, inpatient), severity of the disease, methodology for collecting information and type of study performed, among other factors.
Unlike other viral infections, sequelae have been described that affect the quality of life of persons diagnosed with COVID-19.Table 4shows the time of presentation and type of sequelae, with a predominance of post-COVID syndrome between 21 to 30 days after the acute presentation (85.3%) followed by 31 to 45 days (12.6%). Likewise, respiratory sequelae predominated (61%) followed by musculoskeletal and neurological sequelae (43.1% and 20.0%) respectively. In some studies, fatigue, dyspnea, memory, concentration, attention and sleep disturbances have been described among the symptoms after acute COVID.(30,33)
Among the respiratory sequelae, dyspnea predominated in 49 persons of both sexes and dorsalgia among the musculoskeletal sequelae (75.8% in women and 24.2% in men). Headache was present in 50% of persons of both sexes who reported neurological sequelae, followed by impairment of the senses of smell and taste. Psychological sequelae were reported only by men (anguish, depression), although we consider that there may have been underreporting or that the mental component is not taken into account when symptoms are reported by those affected (Table 5).
According to Bouza E et al(28)the most common persistent post COVID-19 symptoms are dyspnea, cough and chest pain, dyspnea was present in more than 40% of patients(32)especially in those who had severe respiratory failure or were in ICU, but it is also described in up to 15% of patients who had mild or moderate COVID-19.(34)Persistent cough has been described in more than 20% of post COVID-19 cases and chest pain between 5 - 10%.(28)
Regarding osteomuscular symptoms or signs post COVID-19, the predominant musculoskeletal manifestations are arthralgias, myalgias, muscle cramps and contractures, dorsalgia, atrophy and muscle weakness.(28)These clinical findings have been described in different studies.(28,33-35)In the present study, dorsalgia, followed by myalgias, arthralgias and muscle weakness were the main findings (Table 5).
The COVERSCAN study(35)evaluated a prospective cohort of 201 patients four months after discharge from COVID-19. The most common symptoms were fatigue (98%), muscle pain (87%), dyspnea (88%) and headache (83%). In the present study, the neurological manifestations post COVID-19 were headache (50% in both sexes) followed by alterations in taste and smell, alone or in combination.
The COMEBAC study(36)analyzed post-COVID-19 sequelae in a cohort four months after hospital discharge. They found predominance of fatigue (31%), cognitive difficulties (21%) dyspnea (16%) and sleep disorders. In the subgroup of patients who had been admitted to the ICU(94), 23% reported symptoms of anxiety; 18%, depression and 7%, post-traumatic stress disorder.(36)in the present study very few people, all male, reported symptoms such as anxiety and depression. We believe that mental health problems are more prevalent than reported and that there may also be underreporting since mental symptoms are not inquired about in the post-COVID-19 clinical picture.
Post-COVID-19 sequelae are multiple and include physiological, psychological and economic health consequences. COVID-19 disease also has a similar clinical presentation; acute symptoms (fever, cough and dyspnea), followed by pneumonia and bilateral interstitial inflammatory involvement.(9)Among the physiological sequelae, especially those of immediate consequences, respiratory syndromes are described which, in turn, are the most durable (Figure 1). As part of the pathophysiological process of COVID-19 infection, a cytokine storm is activated that initiates the inflammatory response, mainly in the lung. However, the sequelae of this infection are not limited to the respiratory system and have also been reported in the cardiovascular system, central and peripheral nervous system, compromising mental health and leaving sequelae in other organs and systems.(17,28-33)
In approximately one third of the population, pulmonary sequelae of slow recovery develop(9,38)which, in younger patients, are usually repaired, but in older adults scarring in the form of bands or fibrosis is observed at 2-3 weeks post COVID-19. Age and the existence of previous pulmonary disease are considered poor prognostic factors in COVID-19 infection,(38)findings that contribute to determine the duration time of the sequela (Figure 1) to establish an effective and efficient strategy in the follow-up of this type of patients; very relevant, since in some cases an unfavorable short and long term evolution of the pulmonary lesion and a high risk of mortality and morbidity could develop.
Vital capacity is diminished with diseases that damage the lung parenchyma or generate pulmonary restriction such as asthma, chronic obstructive pulmonary disease or in cases of bronchial hyperresponsiveness, as in patients with viral infections, including COVID-19.(37)In this sense, spirometry has proven to be useful to evaluate post-COVID-19 pulmonary sequelae, since the ratio of forced expiratory volume in the first second/forced vital capacity (FEV1/FVC) will be lower as the airway is affected in diseases. In the present study, control spirometry showed that only 7.4% of patients who manifested persistent dyspnea as a post-COVID-19 sequela presented a mild restrictive pattern. These patients belonged to the age group 41 to 50 years, female sex and had arterial hypertension/obesity and hypothyroidism as comorbidity (Table 7). The result could be due to the time elapsed between the onset of the post-COVID-19 sequela and the time when spirometry was performed.
As a limitation, it was difficult to follow up the cases in person because this implied summoning them to the hospital, so telephone follow-up and virtual control consultation were chosen.
Due to delays in the logistical processes for contracting spirometry services, many participants did not come to take this test.
CONCLUSIONS
Of the total number of patients with this diagnosis, only 28.48% showed comorbidity.
The most frequent comorbidity was represented by arterial hypertension (25.53%) with a female predominance.
The predominant age group of patients with COVID-19 was over 40 years of age.
28.8% of COVID-19 patients reported having sequelae.
The predominant sequelae were respiratory, musculoskeletal, and neurological. Dyspnea, dorsalgia, and headache were the most frequent sequelae in each system referred to.
Acknowledgments
Our thanks to Hospital I Florencia de Mora in the person of its Director, Dr. Verónica Sito for accepting the request to carry out the project and providing the facilities and access to the required information.
REFERENCES
1. Ruiz A, Jiménez M. SARS-CoV-2 y pandemia del síndrome respiratorio agudo (COVID-19). Ars Pharm 2020;61(2):63-79. DOI:10.30827/ars.v61i2.15177 [ Links ]
2. Marcial J. El SARS-CoV-2 y otros virus emergentes y su relación con la inocuidad en la cadena alimentaria. Scientia Agropecuaria. 2020;11(2): 267 - 277 Disponible en:https://revistas.unitru.edu.pe/index.php/scientiaagrop/article/view/2929/3095 [ Links ]
3. Cobas-Planchez L, Mezquia-de-Pedro N, Armenteros-Terán S. Características clínicas de pacientes con sospecha de COVID-19 ingresados en el hospital "Frank País García", La Habana. Revista Electrónica Dr. Zoilo E. Marinello Vidaurreta. 2020;45(4). [ Links ]
4. Sepúlveda V, Waissbluth S, González C. Anosmia y enfermedad por Coronavirus 2019 (COVID-19): ¿Qué debemos saber? Rev Otorrinolaringol Cir Cabeza Cuello. 2020; 80: 247-258. DOI: 10.4067/S0718-48162020000200247 [ Links ]
5. Carod-Artal F. Complicaciones neurológicas por coronavirus y COVID-19. Rev Neurol. 2020; 70:311-322.DOI: 10.33588/rn.7009.2020179 [ Links ]
6. Parra V, Flórez C, García F, Romero C. Síntomas gastrointestinales en la enfermedad por COVID-19 y sus implicaciones en la enfermedad Inflamatoria Intestinal. Rev Colomb Gastroenterol. 2020;35(1). DOI: 10.22516/25007440.532 [ Links ]
7. Hama Amin BJ, Kakamad FH, Ahmed GS, Ahmed SF, Abdulla BA, Mohammed SH, et al. Post COVID-19 pulmonary fibrosis; a meta-analysis study. Ann Med Surg. 2022; May;77:103590. doi: 10.1016/j.amsu.2022.103590. [ Links ]
8. Yu M, Liu Y, Xu D, Zhang R, Lan L, Xu H. Prediction of the Development of Pulmonary Fibrosis Using Serial Thin-Section CT and Clinical Features in Patients Discharged after Treatment for COVID-19 Pneumonia. Korean J Radiology. 2020;21(6):746-55. DOI: 10.3348/kjr.2020.0215 [ Links ]
9. Shi H, Han X, Jiang N, Cao Y. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. Lancet Infect Dis. 2020;20(4):425-434. [ Links ]
10. Mitrani RD, Dabas N, Goldberger JJ. COVID-19 cardiac injury: Implications for long-term surveillance and outcomes in survivors. Heart Rhythm. 2021; 17(11):1984-1990. DOI: 10.1016/j.hrthm.2020.06.026. [ Links ]
11. Sardari A, Tabarsi P, Borhany H, Mohiaddin R, Houshmand G. Myocarditis detected after COVID-19 recovery. Eur Heart J Cardiovasc Imaging. 2021;22(1):131-132. doi: 10.1093/ehjci/jeaa166. [ Links ]
12. Parra JE, Duque-Montoya D, Peláez-Félix JC. El COVID-19 también afecta el sistema nervioso por una de sus compuertas: El órgano vascular de la lámina terminal y el nervio olfatorio. Alerta neurológica, prueba de disosmia o anosmia puede Ayudar a un diagnóstico rápido. Int. J. Odontostomat. 2020; 14( 3 ): 285-287. http://dx.doi.org/10.4067/S0718-381X2020000300285 [ Links ]
13. Castellon R, Bender J, Velazquez L. Afectación del sistema nervioso por la COVID-19. Anales de la Academia de Ciencias de Cuba. 2020. Disponible en: http://www.revistaccuba.sld.cu/index.php/revacc/article/view/760/790 [ Links ]
14. Moreno D, Arevalo M, Freire A, Garcia R, Santibañez R. Manifestaciones Neurológicas Asociadas a la Infección Por SARS-CoV-2: Una neuro-revisión de COVID-19, Rev Ecuat Neurol 29, 1, 2020. Disponible en: http://revecuatneurol.com/magazine_issue_article/neurologic-manifestations-sarscov2-infection-neuro-review-covid-19-manifestaciones-neurologicas-infeccion-sarscov2-neuro-revision-covid-19/ [ Links ]
15. Carfì A, Bernabei R, Landi F. For the Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020;324(6):603-5. Disponible en: https://doi.org/10.1001/jama.2020.12603 [ Links ]
16. Xiong Q, Xu M, Li J, Liu Y, Zhang J, Xu Y, Dong W. Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clin Microbiol Infect. 2021;27(1):89-95. doi: 10.1016/j.cmi.2020.09.023. Epub 2020 Sep 23. PMID: 32979574; PMCID: PMC7510771. [ Links ]
17. OPS. (2020). Alerta epidemiológica: complicaciones y secuelas del COVID-19. Disponible en https://www.paho.org/es/documentos/alerta-epidemiologica-complicaciones-secuelas-por-covid-19-12-agosto-2020 [ Links ]
18. MINSA. COVID-19 en el Perú. Sala situacional al 15/11/2021. Disponible en: https://covid19.minsa.gob.pe/sala_situacional.asp [ Links ]
19. Tejada-López Y, Goicochea-Ríos E, Guzmán-Aybar O. Características clínico epidemiológicas de pacientes con diagnóstico de SARS-CoV-2. Hospital I Florencia de Mora ESSALUD-La Libertad, 2020. Disponible en: https://revistas.urp.edu.pe/index.php/RFMH/article/view/3609/5242 [ Links ]
20. MINISTERIO DE SALUD Y PROTECCIÓN SOCIAL. Gestión de las intervenciones individuales y colectivas para la promoción de la salud y prevención de la enfermedad. Lineamientos para el uso de pruebas moleculares RT-PCR, pruebas de antígeno y pruebas serológicas para SARS-CoV-2 (COVID-19) en Colombia. Bogota[Internet]-2021[citado 22 Febrero 2022].Disponible en: https://www.minsalud.gov.co/Ministerio/Institucional/Procesos%20y%20procedimientos/GIPS21.pdf [ Links ]
21. Gutiérrez-Tudela JW. La pandemia de la COVID-19 en el Perú: análisis epidemiológico de la segunda ola. Rev Soc Peru Med Interna. 2021;34(4):129-130.DOI: https://doi.org/10.36393/spmi.v34i4.627 [ Links ]
22. MINSA. COVID-19 en el Perú. Sala situacional al 15/11/2021. Disponible en: https://covid19.minsa.gob.pe/sala_situacional.asp [ Links ]
23. Villagrán-Olivas K, Torrontegui-Zazueta L,Entzana-Galindo A. Características clínico-epidemiológicas de pacientes de COVID-19 en un Hospital de Sinaloa, México. Rev Med UAS.2020;10 (2): 65-79. Disponible en http://dx.doi.org/10.28960/revmeduas.2007-8013.v10.n2.003 [ Links ]
24. Ruiz Cantero M. Las estadísticas sanitarias y la invisibilidad por sexo y de género durante la epidemia COVID-19. Gaxeta Sanitaria. 2021; 95-98; DOI: 10.1016/j.gaceta.2020.04.008 [ Links ]
25. Cortés AE, García Ubaque JC, Becerra CE. Comportamiento por sexo y género de la pandemia de COVID-19 en Colombia. Rev Salud Pública.2020;22(6):1-7. Disponible en: https://revistas.unal.edu.co/index.php/revsaludpublica/article/view/88913 [ Links ]
26. Balboa CT, Lopez J, Muñoz NS, Concha C, Oñat M, Briones J. Comorbilidades asociadas al riesgo de morir por COVID-19 en una cohorte de pacientes ingresados a un hospital de alta complejidad. Medwave 2021;21(S2):eSP25 doi:10.5867/Medwave.2021.S2.SP25 [ Links ]
27. Plasencia-Urizarri TM, Aguilera-Rodríguez R, Almaguer Mederos LE. Comorbilidades y gravedad clínica de la COVID-19: revisión sistemática y meta-análisis. Rev Haban Cienc Méd. 2020; 19(0):[aprox. 0 p.]. Disponible en: http://www.revhabanera.sld.cu/index.php/rhab/article/view/3389 [ Links ]
28. Bouza E, Cantón Moreno R, De Lucas Ramos P, García-Botella A, García-Lledó A, Gómez-Pavón J. Síndrome post-COVID: Un documento de reflexión y opinión. Rev Esp Quimioter 2021;34(4): 269-279. doi:10.37201/req/023.2021. Disponible en https://seq.es/wp-content/uploads/2021/04/bouza20apr2021.pdf [ Links ]
29. Greenhalgh T, Knight M. Long COVID: A Primer for Family Physicians. Am Fam Physician. 2020;102(12):716-7. PMID: 33320511 [ Links ]
30. Del Rio C, Collins LF, Malani P. Long-term Health Consequences of COVID-19. JAMA. 2020;324(17):1723-1724. DOI: 10.1001/jama.2020.19719 [ Links ]
31. Carfì A, Bernabei R, Landi F. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020: 324(6):603-605 DOI: 10.1001/jama.2020.12603 [ Links ]
32. Chopra V, Flanders SA, O'Malley M, Malani AN, Prescott HC. Sixty-Day Outcomes Among Patients Hospitalized With COVID-19. Ann Intern Med. 2021 Apr;174(4):576-578. doi: 10.7326/M20-5661. Epub 2020 Nov 11. PMID: 33175566; PMCID: PMC7707210. [ Links ]
33. Carod-Artal F. Síndrome post-COVID19: epidemiología, criterios diagnósticos y mecanismos patogénicos implicados. Rev Neurol. 2021;72:384-396. DOI: https://doi.org/10.33588/rn.7211.2021230 [ Links ]
34. De Lorenzo R, Conte C, Lanzani C, Benedetti F, Roveri L, Mazza MG, et al. Residual clinical damage after COVID-19: A retrospective and prospective observational cohort study. PLoS One. 2020;15(10):e0239570. DOI: 10.1371/journal.pone.0239570. Disponible en https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0239570 [ Links ]
35. Dennis A, Wamil M, Alberts J, Oben J, Cuthbertson DJ, Wootton D, et al; COVERSCAN study investigators. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ Open 2021; 11: e048391. [ Links ]
36. Morin L, Savale L, Pham T, Colle R, Figueiredo S, Harrois A, et al. Writing committee for the COMEBAC Study Group. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA. 2021;325(15):1525-1534. doi:10.1001/jama.2021.3331 [ Links ]
37. Chérrez-Ojeda Iván, Gochicoa-Rangel Laura, Salles-Rojas Antonio, Mautong Hans. Seguimiento de los pacientes después de neumonía por COVID-19. Secuelas pulmonares. Rev Alerg Méx. 2020; 67( 4 ): 350-369, https://doi.org/10.29262/ram.v67i4.847. [ Links ]
38. Molina-Molina M. Secuelas y consecuencias de la COVID-19. Medicina respiratoria 2020, 13 (2): 71-77. Disponible en http://www.neumologiaysalud.es/descargas/R13/R132-8.pdf [ Links ]
Funding sources: This project was funded by the Universidad César Vallejo through the support system for teaching research 2021.
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: February 03, 2022; Accepted: August 17, 2022











 texto en
texto en