Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.4 Lima oct./dic. 2022 Epub 12-Oct-2022
http://dx.doi.org/10.25176/rfmh.v22i4.4762
Clinical case
Gastric Adenomyoma in adult a Case Report
1Hospital Nacional Edgardo Rebagliati Martins. Lima - Perú.
2Facultad de Medicina, Universidad Nacional Mayor de San Marcos.
3Hospital Nacional Daniel A. Carrión, Callao, Perú.
Clinical case:
We present a 52 years old man who attended the emergency room due pyloric syndrome and who underwent a distal gastrectomy. The pathological report revealed a gastric adenomyoma with ulcerative lesion.
Discussion:
This pathology is an unusual finding, and the literature describe it with extremely low rate of malignant transformation.
Conclusion:
Gastric adenomyoma is a infrequent pathology and should be taken into account when endoscopic studies are not enough to determine the etiology of a pyloric syndrome.
Keywords: Adenomyoma; Stomach; Pylorus. (Source: MeSH NLM).
INTRODUCTION
Gastric adenomyoma is a rare benign pathology characterized by ducts and glands surrounded by smooth muscle stroma1-5. The ages of presentation are variable, presenting from neonates to the elderly2. 52 cases have been described in the literature up to 20171,4. The most frequent age of presentation is between the fourth and sixth decades of life1,4without gender predilection1and may be associated with annular pancreas, Gardner syndrome with duodenal adenomas and gastric duplication1. The clinical presentation is variable, and may include nausea, vomiting, epigastric pain, even hematemesis, anemia and melena1,3,4. Despite being considered a benign disease, cases of malignant transformation have been described in up to 2%4. The importance of taking this pathology into account lies above all when the endoscopic findings are inconclusive in the presence of pyloric syndrome that does not show malignant disease or other types of obvious obstructive lesions.
CLINICAL CASE
A 52-year-old male, natural from Iquitos, with no relevant history, goes to the emergency room reporting 3 days of epigastric pain, nausea, vomiting and the inability to eliminate flatus for 2 days; also loses weight of 7kg in 1 month and oral intolerance to solids and liquids; also, increased appetite. Examination shows marked distension of the upper abdomen with tympanism, without peritoneal reaction; A simple abdominal X-ray was performed, showing great dilatation of the gastric chamber with no signs of lower intestinal obstruction or air-fluid levels. It is concluded that the patient presents emesis due to a pyloric syndrome to rule out an infiltrative lesion; hospitalization is indicated to complete studies.
The total abdominal tomography with intravenous contrast evidenced: stomach with distention and food content inside, impresses conditioned by an obstructive process located at the pyloric level that is thickened up to 16mm with diffuse mucosal enhancement of probable inflammatory cause, the adjacent fat shows diffuse striation ; concluding mural thickening at the level of the pyloric region with diffuse mucosal enhancement conditioning gastric obstructive process, consider high suspicion of inflammatory process, the possibility of neoplastic infiltrative process is not discard.
An upper gastrointestinal endoscopy was performed where a linear ulcer with regular edges and a fibrinous bed was described at the level of the gastric angle, which were biopsied, as well as deformed antrum due to healing of the lesser curvature ulcer, pylorus occluded due to healing of the lesser curvature ulcer. Duodenal bulb and second duodenal portion not observed; gastric ulcer was concluded that deforms and occludes pylorus without signs of active bleeding. The pathological anatomy described severe active plasmacytic chronic gastritis with edema and fibrosis of the lamina propria, regenerative epithelium with mild dysplasia, necrotic ulcer fundus with shadow cells.
Preoperative studies describe: Leukocytes 8.03x103/uL, Hemoglobin 12.1g/dL, Platelets 320x103/uL, blood group O positive, Albumin 4.1g/dL, Creatinine 0.69mg/dL, Glucose 94mg/dL, Urea 41.2mg/dL.
After the endoscopic studies and the pathological anatomy reports do not conclude the etiology of the pyloric syndrome, it is decided to perform a Radical Distal Gastrectomy with D2 Lymphadenectomy with reconstruction by Y Roux Gastrojejunostomy due to a pre-pyloric gastric inflammatory process that conditions partial obstruction of the pylorus, where the possibility of a neoplastic infiltrative process is not ruled out. The findings showed a pre-pyloric gastric tumor with lesser curvature of 4x3cm in diameter, hard that occludes and compresses the pylorus, with serosal retraction of the posterior gastric wall that conditions gastric chamber dilatation. No liver or peritoneal lesions or free fluid. After the surgical procedure, the patient evolved favorably and was discharged on the eleventh postoperative day with good oral tolerance.
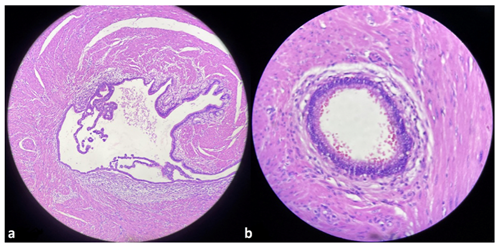
The pathological anatomy report of the operative piece described: Gastric adenomyoma with multiple ulcerative lesion, fibrosis and serosal retraction with hypertrophic arterial vessels that reach the submucosa (Figure 1) Peri-ulcerative regenerative epithelium and granulation tissue with isolated giant cells of the foreign body type . Chronic follicular gastritis with follicular mantle hyperplasia, free surgical margins - free omentum, free perigastric lymph nodes 0/26 with adenitis and lymphatic congestion.
DISCUSSION
Gastric adenomyoma is a rare benign lesion composed of ducts and glands surrounded by smooth muscle stroma1-5. Also known as myoglandular hamartoma, adenomyomatous hamartoma or myoepithelial hamartoma2,3,5. It is usually found in the antrum and pylorus and, when the adenomyoma is extragastric, it is located in the duodenum and jejunum. For several authors, the location of adenomyomas is gastric (25-38%), duodenum (17-36%) and jejunum (15-21%), and the location in the stomach is: antrum (85%), pylorus (15% )1,3and exceptionally in the body1.
Magnus Alsleben was the first to describe this entity in 1903, the product of 5 cases found incidentally in necropsies5. Various authors consider this entity to be a hamartoma while others consider it a variant of a heterotopic pancreas1,2. In some cases it coexists with heterotopic pancreas and in other cases it shows communication between the gastric lumen and the epithelial component of the lesion1.
In 1909, Heinrich described 3 histological subtypes of heterotopic pancreas, considering the third type as “adenomyoma”, while Matsushita described his echoendoscopic findings and related them to Heinrich's description as follows1:
Type 1: Exocrine and Endocrine Pancreas (Heterotopic Pancreas); Echo endoscopy shows indistinct margins, heterogeneous appearance and location between the third and fourth layers.
Type 2: Exocrine Pancreas without islets (Heterotopic Pancreas); echo endoscopy shows similar to type 1 but localization only in the third layer.
Type 3: Only ducts (adenomyoma); Echo endoscopy shows a small anechoic nucleus with thickening of the fourth layer.
The ages of presentation are variable, with the youngest patient being a 1-week-old neonate and the oldest being an 81-year-old person2; To date, 52 cases have been described in the literature up to 20171,4with the most frequent age of presentation being between the fourth and sixth decade of life1,4with no gender predilection1. Associated conditions may include annular pancreas, Gardner syndrome with duodenal adenomas, and gastric duplication1.
The clinic is diverse, and can range from the asymptomatic which are discovered during a laparoscopy or necropsies1,3, with the most reported cases being those associated with non-specific symptoms such as nausea, vomiting, epigastric pain, hematemesis, anemia, melena1,3,4and even reaching intermittent pyloric obstruction3. Likewise, cases of secondary peritonitis due to perforation have been described. Making a preoperative diagnosis is difficult, because most of the symptoms are not specific, in addition to the few cases described in the literature1,3.
For diagnosis, endoscopy is not usually very effective because it manifests as a submucosal lesion, in addition to not being able to differentiate between hamartoma and leiomyoma, melanoma, lymphoma, carcinoid tumor, Kaposi's sarcoma, GIST or eosinophilic granuloma3. For which, all these injuries must end up in surgical management to ensure a correct diagnosis2-4.
Despite being considered a benign lesion, the potential for malignant transformation does exist1-3being less than 2%4. The literature has described a case of gastric adenomyosis with malignant transformation of its glandular center2. The use of endoscopic technologies for the resection of this type of lesion has not been reported; however, in retrospective studies it has been determined that these lesions have been resected using this technique without further complications2,4. Most of the reviewed series indicate the open or laparoscopic surgical approach as the ideal management option.
CONCLUSIONS
Gastric adenomyoma is a rare benign pathology, difficult to diagnose clinically, which is usually diagnosed after the study of surgical specimens. It should be considered as a diagnostic presumption when previous studies are inconclusive; likewise, surgical management should not be delayed due to a lack of etiology, since this can generate unnecessary delays that could lead to clinical deterioration in patients.
REFERENCES
1. Duran MA, Gómez JR, Guerra T. Gastric Adenomyoma: The Unexpected Mimicker. GE Port J Gastroenterol. 2017 Jul;24(4):198-202. DOI: 10.1159/000453302. [ Links ]
2. Wang S, Cao H, Zhang Y, Xu M, Chen X, Piao M, Wang B. Endoscopic submucosal dissection for gastric adenomyoma: A rare entity of 15 cases among 571 patients with gastric submucosal eminence lesions. Medicine (Baltimore). 2017 Mar;96(9):e6233. DOI: 10.1097/MD.0000000000006233. [ Links ]
3. Nabi J, Authoy FN, Akhter SM. Atypical presentation of myoepithelial hamartoma in the antrum of the stomach, mimicking a gastrointestinal stromal tumor: a case report. J Med Case Rep. 2012;6:382. DOI: 10.1186/1752-1947-6-382. [ Links ]
4. Anand S, Dhua AK, Bhatnagar V, Agarwala S, Kandasamy D, Kakkar A. Gastric Adenomyosis: A Rare Cause of Pyloric Mass in Children. J Indian Assoc Pediatr Surg. 2020;25(3):172-174. DOI: 10.4103/jiaps.JIAPS_44_19. [ Links ]
5. Lasser A, Koufman WB. Adenomyoma of the stomach. Am J Dig Dis. 1977 Nov;22(11):965-9. DOI: 10.1007/BF01076194. [ Links ]
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: February 09, 2022; Accepted: July 27, 2022











 texto en
texto en