Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.4 Lima oct./dic. 2022 Epub 12-Oct-2022
http://dx.doi.org/10.25176/rfmh.v22i4.4751
Clinical case
Near-fatal asthma as clinical manifestation in onset diabetic patient: Case report
1Facultad de medicina. Universidad Nacional de Trujillo. Trujillo, Perú.
2Instituto Regional de Enfermedades Neoplásicas. Trujillo, Perú.
3Hospital Belén de Trujillo. Trujillo, Perú.
Introduction:
Near-fatal asthma (NFA) is defined as the most severe form of asthma characterized by a refractory asthma attack with an arterial carbon dioxide tension (PaCO2) greater than 45 mmHg and altered consciousness, requiring mechanical ventilation.
Clinical Case:
We reported the case of 40-year-old female patient, obese and asthmatic with irregular treatment who presented dyspnea accompanied by severe oppressive chest pain and loss of consciousness, with generalized cyanosis and severe shortness of breath, for which she underwent emergency endotracheal intubation and mechanical ventilation. Laboratory tests show decompensated respiratory acidosis, glycemia of 258 mg / dl and HbA1C of 7.94%; her diagnosing diabetes mellitus (DM). The presentation of NFA is rare and as a clinical manifestation in an obese patient with onset diabetic has never been reported in Peru; therefore, asthmatic patients with obesity and DM should be monitored due to the susceptibility to develop NFA.
Keywords: Asthma; Diabetes mellitus; Mechanical ventilation. (fuente: MeSH NLM).
INTRODUCTION
Near-fatal asthma (NFA) is an inflammatory disease of the respiratory system in which a conventional therapeutic approach has failed, it is characterized by a refractory asthmatic crisis with a partial pressure of carbon dioxide (PaCO2) greater than 45 mmHg, consciousness level alteration, and mechanical ventilation requirement1,2. NFA affects 5 out of 100,000 asthma patients per year globally1. In Peru, there have been no studies at the national level on the clinical-epidemiological characteristics of asthmatic patients who arrive at emergency areas3. However, a study conducted at the Daniel Alcides Carrión National Hospital found that the annual incidence of patients who met the criteria for near-fatal asthma was 4 per 1,000 hospitalized patients diagnosed with asthma4.
Several risk factors for death related to asthma have been identified, such as a history of previous intubation, ICU stay, multiple emergency visits during the previous year, abuse of beta-agonist drugs, respiratory tract infections, sensitivity to aeroallergens, age, respiratory tract infections, systemic dependence on glucocorticoids5-7. Similarly, diabetes mellitus is also a risk factor with great relevance in recent years due to its high incidence worldwide and common comorbidity in asthmatic patients8,9.
The mechanisms that explain the exacerbation of asthma in diabetic patients are not yet fully elucidated, it is hypothesized that low-grade systemic inflammation and hyperglycemia are key points for their understanding9-11. Although the coexistence of asthma and diabetes mellitus in the same patient is frequent, there is little information worldwide and none in Peru on near-fatal asthma as a clinical manifestation in diabetic patients, therefore, the aim of this work is to describe the clinical picture in a case of near-fatal asthma as a clinical manifestation in a debut diabetic patient for its recognition in the emergency area and to carry out an adequate therapeutic approach.
DESCRIPTION OF THE CLINICAL CASE
A 40-year-old female patient with incomplete high school, from Moche who works in outpatient commerce, has had asthma for 10 years with irregular treatment, with no family history of the disease. In laboratory tests, he has an arterial blood gas study, he also has type I obesity (BMI: 30) and uncontrolled arterial hypertension. She has history of COVID-19 a year ago and a dust allergy; In addition, her mother was diagnosed with prediabetes approximately 8 years ago.
One week before going to the emergency room and being hospitalized, she presented dyspnea with an insidious onset and a progressive course, generally in the afternoons and at night, which limits her ability to carry out her daily activities and worsens due to exposure to humidity, cold, and the realization of higher efforts. During that week, she presented 3-4 shortness of breath crises a day and went to a medical center near his home to have nebulizations performed.
One day before admission, she suffered crises of acute dyspnea with little effort that did not improve with inhaled salbutamol. In the emergency service, she was admitted with dyspnea accompanied by signs of respiratory distress, poor general condition and an oxygen saturation of 85%, oppressive retrosternal chest pain of severe intensity and generalized cyanosis, disorder of consciousness, snoring in the middle ⅓ and bases of both hemithorax with a predominance of right hemithorax, rhythmic and regular heart sounds. Information on emergency baseline pulmonary function tests could not be obtained.
A few minutes after her emergency stay, she presented a sudden loss of consciousness where a respiratory arrest was identified, for which emergency endotracheal intubation was performed, she was transferred to perform a chest X-ray (Figure 1) and then received support with mechanical ventilation plus sedoanalgesia. A RT-PCR test for SARS-CoV-2 was requested with a negative result and laboratory tests (Table 1). Arterial blood gas analysis (AGA) revealed decompensated respiratory acidosis and hyperglycemia; Furthermore, a high value was obtained in the glycosylated hemoglobin test, for which she was diagnosed with type 2 diabetes mellitus (DM2), decompensated by hyperglycemia. The patient does not present with complications of ketoacidosis or hyperosmolar state, an interconsultation with the ICU was carried out for management in that service; however, it did not have beds available.
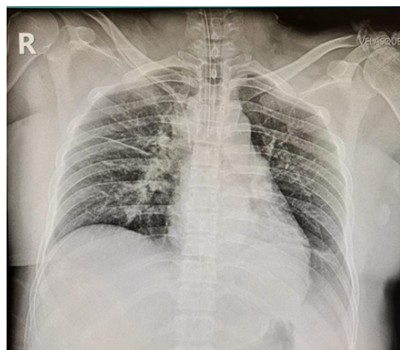
Figure 1 Simple anteroposterior projection chest X-ray. Interstitial congestion pattern (Kerley lines), prominence of the pulmonary arterial arch, accentuated bronchovascular pattern, presence of an endotracheal tube with a distal tip projecting close to the carina and a right-access central venous catheter with a distal tip projecting into the superior vena cava
Table 1. Laboratory tests on admission.
| PARAMETER | RESULT | NORMAL VALUES |
|---|---|---|
| pH | 7,29 | 7,35-7,45 |
| PCO2 (mmHg) | 49,8 | 35-45 |
| PO2 (mmHg) | 54,4 | 80-100 |
| HCO3 (mEq) | 24,2 | 20-24 |
| SatO2 (%) | 89,4 | 95-100 |
| Glu (mg/dl) | 258 | 70-99 |
| HbA1C (%) | 7,94 | <5,7 |
The next day, the patient remains in support with mechanical ventilation and sedoanalgesia; Physical examination shows absence of breath sounds (silent lung). Subsequently, he received inhalations of bronchodilators by MDI (Metered Dose Inhaler) and corticosteroid therapy. Magnesium sulfate was used as a complement to first-line therapy, to which it did not present a favorable response, so ketamine, norepinephrine, insulin infusion therapy, and antibiotic therapy (ceftriaxone, clindamycin) were indicated due to the suspicion of a bacterial infectious process. over aggregated.
In the subsequent days, during his stay on mechanical ventilator support under the aforementioned conditions, she presented an unfavorable evolution with hemodynamic instability, laboratory tests (Table 2), and high suspicion of pneumonia associated with mechanical ventilation, for which reason the rotation of antibiotics to Carbapenems (Meropenem). After 4 days with the change of antibiotic therapy, she presents a slight ventilatory and hemodynamic improvement, a tracheostomy was performed, after which she was weaned and taken off the mechanical ventilator after 14 days. Later, she is transferred to hospitalization to complete treatment, and from where she is discharged after 20 days.
Table 2. Laboratory tests during evolution in relation to treatment
| Exams | Evolution throughout days | ||||
|---|---|---|---|---|---|
| 3 hours later | Day 2 | Day 3 | Día 4 | Day 25 | |
| Fi02(%) | 100% | 80% | 45% | 45% | 21% |
| pH | 7,01 | 6,98 | 7,28 | 7,07 | 7,44 |
| PCO2 (mmHg) | 145,9 | 158 | 60,5 | 107,9 | 38,7 |
| PO2 (mmHg) | 208,2 | 79,4 | 88,2 | 90,8 | 77,8 |
| HCO3 (mEq) | 37,4 | 38 | 29,3 | 31,9 | 26,6 |
| SatO2 (%) | 99,0 | 83,7 | 95,2 | 91,4 | 95,9 |
| Gluc (mg/dl) | 264 | 252 | 222 | 185 | 205 |
| PaFiO2 | 208,2 | 158,8 | 220,4 | 201,9 | 311 |
| K+ (mEq/L) | 5,6 | 6,69 | 4,76 | 6,34 | 3,42 |
| BUN(mg/dl) | 18 | 22 | 27 | 32 | 14 |
DISCUSSION
Near-fatal asthma defines a subset of patients with asthma who are at increased risk of death from their disease12. Studies show that deaths from asthma attacks typically occur in patients with poorly controlled asthma whose condition gradually deteriorates over days or weeks before the fatal or near-fatal episode of asthma occurs13. The signs and symptoms that were evidenced in the patient were decreased consciousness level, respiratory distress, cyanosis, auscultatory silence, SatO2 of 89.4% (<90%), PaO2 of 54.4 mmHg (<60 mmHg) and PaCO2 of 49.8 mmHg (>45mmHg), which are consistent with the clinical manifestations of NFA, which could have led to the development of respiratory arrest1,6,12.
As usual management of NFA, immediate ventilatory support is given to preserve adequate oxygenation, reduce dynamic hyperinflation and reduce probable hypercapnia (confirmed in the AGA); and subsequently administer nebulized B2-agonists, systemic corticosteroids, theophylline, ketamine, or epinephrine, which relieve airflow with reduction of airway obstruction and mucus; depending on the situation6,14. In this case, the patient was refractory to salbutamol nebulization before admission to the emergency room; After endotracheal intubation and mechanical ventilation, there was no favorable response to magnesium sulfate, so ketamine, norepinephrine, and vasopressors were indicated, described as part of non-conventional therapy6.
Several risk factors were identified in this patient, such as low socioeconomic status, irregular treatment of asthma, difficulty in perceiving the severity of her symptoms, and ignorance of the condition of DM2 by the patient and her relatives; which together led to their high risk of death.
Among these factors, DM2 stands out due to its association with worsening asthma control, increasing the chances of exacerbations, complications and hospitalizations10,11. The hypothesis of its association is based on low-grade systemic inflammation, characterized by high levels of inflammatory markers such as IL-6 and TNF-alpha that favor the differentiation of Th2 cells into Th17 and the production of high levels of IL-17 that are seen in severe asthma; as well as in obese people and those with DM2, conditions present in this patient10,15,16. Besides, hyperglycemia generates advanced glycation end products that can affect microvascular structures such as the alveolar capillary network in the lung; which reduces lung function and decreases lung capacity10.
Additionally, research has found a decreased risk of hospitalizations for asthma in diabetic patients who have regular treatment with metformin16,17, which contributes to the explanation of the almost fatal asthma in this case, since being a debut diabetic patient did not have a treatment before admission.
Despite the precipitating factors for NFA already mentioned and according to the study conducted by Sandrock C, et al.18, viral infections represented 59% of the patients, with rhinovirus, particularly human rhinovirus-C, being the Most common causative agent detected 5 days prior to asthma exacerbation. Other viruses that cause this complication are also mentioned, such as respiratory syncytial virus (RSV) type A and B, as well as influenza A, which seem to be the most frequent and recurrent threats. In this case, the viral infection by rhinovirus could explain the manifestation of almost fatal asthma in the patient; even more, having diabetes mellitus which generates immunosuppression. However, a severe bacterial infection that is not secondary to a viral infection would be unlikely to cause near-fatal asthma.
The patient did not show symptoms of viral infection days before emergency admission; In addition, no diagnostic tests were performed to rule out the presence of said infection.
In conclusion, the presentation of NFA is rare and has not been reported in Peru as a clinical manifestation in an obese patient with debut DM; for this reason, asthmatic patients with obesity and DM should be monitored due to the susceptibility to developing an NFA.
REFERENCES
1. Mora C, Urbina Medina, Urbina H, Lobo P, Barreto O. Asma casi fatal. Archivos Venezolanos de Puericultura y Pediatría ENT#091;InternetENT#093;. 2010 ENT#091;citado el 20 de noviembre del 2021ENT#093;;73(3):47-54. Disponible en https://www.redalyc.org/pdf/3679/367936952009.pdf. [ Links ]
2. Doshi V, Shenoy S, Ganesh A, Lankala S, Henkle J. Near Fatal Asthma in an Inner City Population. Am J Ther ENT#091;InternetENT#093;. 2016 ENT#091;citado el 20 de noviembre del 2021ENT#093;; 23(6):1375-1380. DOI: https://doi.org/DOI: 10.1097/MJT.0000000000000152. [ Links ]
3. Cachay J. Evaluación clínico-flujométrica en exacerbaciones agudas de asma bronquial, tratados con Fenoterol, en un Servicio de Emergencia, en adultos ENT#091;Tesis de EspecialidadENT#093;. Perú: Universidad Nacional Mayor de San Marcos; 2015. Disponible en: https://cybertesis.unmsm.edu.pe/bitstream/handle/20.500.12672/13500/Cach ay_Diaz_Jose_Ramiro_2015.pdf?sequence=1. [ Links ]
4. Sánchez K. Asma casi fatal en el Hospital Nacional Daniel Alcides Carrión entre febrero 1998 a febrero 2008. Interciencia ENT#091;InternetENT#093;. 2008 ENT#091;citado el 20 de noviembre del 2021ENT#093;;2(3):10-19. Disponible en: https://www.clinicainternacional.com.pe/pdf/revista-interciencia/4/Articulo_Orig inal2.pdf. [ Links ]
5. Serrano-Pariente J, Plaza V. Near-fatal asthma: A heterogeneous clinical entity. Curr Opin Allergy Clin Immunol ENT#091;InternetENT#093;. 2017 ENT#091;citado el 20 de noviembre del 2021ENT#093;;17(1):28-35. DOI: https://doi.org/10.1097/ACI.0000000000000333. [ Links ]
6. D'Amato G, Vitale C, Lanza M, Sanduzzi A, Molino A, Mormile M, et al. Near fatal asthma: Treatment and prevention. Eur Ann Allergy Clin Immunol ENT#091;InternetENT#093;. 2016 ENT#091;citado el 20 de noviembre del 2021ENT#093;;48:116-22. Disponible en: https://mrmjournal.biomedcentral.com/articles/10.1186/s40248-016-0073-0. [ Links ]
7. D'Amato G, Vitale C, Molino A, Stanziola A, Sanduzzi A, Vatrella A, et al. Asthma-related deaths. Multidiscip Respir Med ENT#091;InternetENT#093;. 2016 ENT#091;citado el 20 de noviembre del 2021ENT#093;;11(1):1-5. DOI: https://doi.org/10.1186/s40248-016-0073-0. [ Links ]
8. Chang Y, Ko H, Lu M, Chpu C, Su K, Hsu C, et al. Independent risk factors for death in patients admitted for asthma exacerbation in Taiwan. Care Respir Med ENT#091;InternetENT#093;. 2020 ENT#091;citado el 20 de noviembre del 2021ENT#093;;30(7). DOI: https://doi.org/10.1038/s41533-020-0164-4. [ Links ]
9. Kosmalski M, Rozycka-Kosmalska M, Witusik A, Pietras T. The coincidence of diabetes mellitus and asthma, their probable causal relationships and therapeutic opportunities. Adv Respir Med ENT#091;InternetENT#093;. 2020 ENT#091;citado el 20 de noviembre del 2021ENT#093;;88:590-598. DOI: https://doi.og/10.5603/ARM.a2020.0168. [ Links ]
10. Marques R, Dos Santos M, Carvalho A, Marques L, Souza-Machado C. Association between Asthma and Type 2 Diabetes Mellitus-A Literature Review. Can Respir J ENT#091;InternetENT#093;. 2021 ENT#091;citado el 20 de noviembre del 2021ENT#093;;Article ID 8830439. DOI: https://doi.org/10.1155/2021/8830439. [ Links ]
11. Khateeb J, Fuchs E, Khamaisi M. Diabetes and Lung Disease: An Underestimated Relationship. Rev Diabet Stud ENT#091;InternetENT#093;. 2019 ENT#091;citado el 20 de noviembre del 2021ENT#093;;15. DOI: https://doi.org/10.1900/RDS.2019.15.1. [ Links ]
12. Sabin B, Greenberger P. Potentially (near) fatal asthma. Allergy Asthma Proc ENT#091;InternetENT#093;. 2012 ENT#091;citado el 20 de noviembre del 2021ENT#093;;33(Supl 1): S44-S46. DOI: https://doi.org/10.2500/aap.2012.33.3546. [ Links ]
13. Restrepo R, Peters J. Near-fatal asthma: recognition and management. Curr Opin Pulm Med ENT#091;InternetENT#093;. 2008 ENT#091;citado el 7 de diciembre del 2021ENT#093;;14:13-23. DOI: https://doi.org/ 10.1097/MCP.0b013e3282f1982d. [ Links ]
14. Bermeo L, Velasco D. Guía para el tratamiento de la crisis asmática. Arc Med Urg Méx ENT#091;InternetENT#093;. 2013 ENT#091;citado el 7 de diciembre del 2021ENT#093;;5(2):60-69. Disponible en: https://www.medigraphic.com/pdfs/urgencia/aur-2013/aur132c.pdf. [ Links ]
15. Carpaji O, van den Berge M. The asthma-obesity relationship: underlying mechanisms and treatment implications. Curr Opin Pulm Med ENT#091;InternetENT#093;. 2018 ENT#091;citado el 7 de diciembre del 2021ENT#093;;24:42-49. DOI: https://doi.org/10.1097/MCP.0000000000000446. [ Links ]
16. Wu T. Diabetes, insulin resistance, and asthma: a review of potential links. Curr Opin Pulm Med ENT#091;InternetENT#093;. 2021 ENT#091;citado el 7 de diciembre del 2021ENT#093;;27:29-36. DOI: https://doi.org/10.1097/MCP.0000000000000738. [ Links ]
17. Wrn L, Zhong W, Chai Y, Zhong Q, Gao J, Guan L, et al. Association of Metformin Use with Asthma Exacerbation in Patients with Concurrent Asthma and Diabetes: A Systematic Review and Meta-Analysis of Observational Studies. Can Respir J ENT#091;InternetENT#093;. 2020 ENT#091;citado el 7 de diciembre del 2021ENT#093;;Article ID 9705604. DOI: https://doi.org/10.1155/2020/9705604. [ Links ]
18. Sandrock C, Norris A. Infection in Severe Asthma Exacerbations and Critical Asthma Syndrome. Clin Rev Allergy Inmunol ENT#091;InternetENT#093;. 2015 ENT#091;citado el 7 de diciembre del 2021ENT#093;:48(1):104-13. DOI: https://doi.org/10.1007/s12016-014-8435-x. [ Links ]
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: February 04, 2022; Accepted: July 16, 2022











 texto en
texto en 


