Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de la Facultad de Medicina Humana
Print version ISSN 1814-5469On-line version ISSN 2308-0531
Rev. Fac. Med. Hum. vol.22 no.4 Lima Oct./Dec. 2022 Epub Oct 12, 2022
http://dx.doi.org/10.25176/rfmh.v22i4.5184
Clinical case
Xanthogranulomatous appendicitis; a diagnostic challenge: Clinical Case
1Unidad Médica de Alta Especialidad Hospital de Especialidades de Puebla Centro Médico Nacional General de División Manuel Ávila Camacho del Instituto Mexicano del Seguro Social, Puebla, Mexico.
2Unidad Médica de Alta Especialidad Hospital de Especialidades de Puebla Centro Médico Nacional General de División Manuel Ávila Camacho del Instituto Mexicano del Seguro Social. Facultad de Medicina, Benemérita Universidad Autónoma de Puebla, Puebla, Mexico.
3Postgrado del área de la Salud, Universidad Popular Autónoma del Estado de Puebla, Puebla, Mexico.
Introduction:
Xanthogranulomatous inflammation is a chronic inflammatory process, rarely located in the appendix. A case of xanthogranulomatous appendicitis is presented.
Clinical case:
A 77-year-old male presents with intermittent pain in the right hemiabdomen and hyperthermia of one month's evolution. Physical examination showed a tumor in the iliac fossa and right abdomen. He underwent surgery for a probable incarcerated right inguinal hernia, acute perforated appendicitis was found, with inflammation and adhesions, purulent fluid in the right hemiabdomen, and abdominal wall dissection. The histopathological result was xanthogranulomatous appendicitis. The evolution of the patient was favorable.
Conclusion:
Xanthogranulomatous appendicitis simulates a typical picture of acute appendicitis. Histopathologically, pathologies such as Crohn's disease, malacoplakia, and tuberculous appendicitis were ruled out.
Keywords: Xanthogranulomatous appendicitis; Appendicitis; Foam cells; Michaelis-Gutmann bodies (Sourse: MeSH NLM).
INTRODUCTION
Acute appendicitis is one of the most common surgical problems in clinical practice. Pathologic evaluation is the gold standard for diagnosing acute appendicitis. Routine histopathologic evaluation is performed to confirm the diagnosis of acute appendicitis and may reveal other important pathologic details.1
Xanthogranulomatous inflammation (XGI) is a chronic inflammatory process observed in other sites such as gall bladder, kidney, ovaries, prostate, epididymis, etc. Appendiceal involvement is quite rare and has been observed more frequently in interval appendicitis. It is characterized by a cluster of xanthoma-like cells, with a prominent histiocytic component.2Microscopically there is ulceration along with numerous inflammatory cells, mostly neutrophils located in the muscularis propria, necrosis, and congestion.
DESCRIPTION OF THE CLINICAL CASE
We present a 77-year-old male patient with a personal pathological history of type 2 diabetes, without specifying the time of evolution or treatment; he referred to a clinical picture of four weeks of evolution with mild abdominal pain predominantly right, unquantified hyperthermia of two days of evolution with antibiotic and symptomatic management. There was a frank improvement for three weeks; but eight days before surgery the symptoms increased, she had an increase in volume at the level of the right iliac fossa with increased local temperature. Physical examination showed a soft abdomen, depressible, painful at the site of the tumor, measuring 15x15cm, of solid consistency, with hyperemic and hyperthermic skin surface and no evidence of peritoneal alarm. The rest of the physical examination was normal with the following vital signs: BP 110/75, HR 78 bpm, RR 19 rpm, axillary temperature 37°C, and O2 saturation 93%.
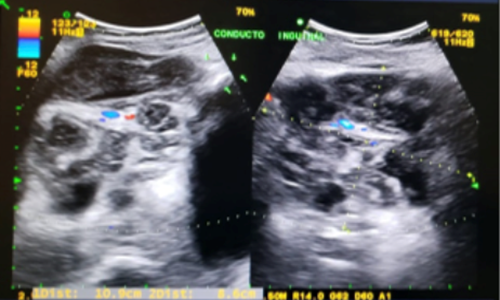
Preoperative laboratory studies showed leukocytosis at the expense of neutrophils, the rest of the blood biometry and coagulation times were normal (Table 1). Ultrasonography (USG) of the abdominal and inguinal wall showed the presence of right inguinal herniaFigure 1.
Table 1. Preoperative clinical studies.
| BLOOD BIOMETRY | |
|---|---|
| RED FORMULA | |
| Hemoglobin(Hb) | 35.1% |
| Platelets | 400x103/uL |
| WHITE FORMULA | |
| Total leukocytes | 15.0x103/uL |
| Total neutrophils | 12,900/uL |
| PARTIAL BLOOD CHEMISTRY | |
| Serum glucose | 185 mg/dl |
| COAGULATION PROFILE | |
| Prothrombin time | 14.5 sec. |
| Control plasma(TP) | 12.2 |
| INR | 1.21 |
The patient underwent exploratory laparotomy and 500ml of fetid purulent material was found in the abdominal wall at the tumor site, in the abdominal cavity intestinal loops adhered to the cecum where plastron and inflamed cecal appendix were found in the distal third with perforation in the middle third. The blood biometry at 72 hours reported a decrease in leukocytes, the result of the culture of the abdominal wall exudate was positive for Streptococcus viridans sensitive to imipinem and clindamycin (Table 2), the histopathological diagnosis was xanthogranulomatous appendicitisFigure 3. The evolution was stable, with improvement and in eight days he was discharged home without any apparent complication.
Tabla 2. Postoperative clinical studies.
| CULTURE OF ABDOMINAL WALL EXUDATE | |
|---|---|
| Bacteriological examination | Streptococcus viridans |
| ANTIBIOGRAM BY DISK DIFUSSION | |
| Imipinem | Sensible |
| Clindamycin | Sensible |
| BLOOD BIOMETRY | |
| RED FORMULA | |
| Hemoglobin(Hb) | 10.7 g/dL |
| Hematocrit | 32.8% |
| Platelets | 407x103/uL |
| WHITE FORMULA | |
| Total leukocytes | 13.5x103/uL |
| Total neutrophils | 89% |
| PARTIAL BLOOD CHEMISTRY | |
| Serum glucose | 152.0 mg/dl |
| Serum urea nitrogen | 15 mg/dl |
| Serum urea | 32.1 mg/dl |
| Serum creatinine | 0.7 mg/dl |
| SERUM ELECTROLYTES | |
| Serum sodium | 139.0 mmol/L |
| Serum potassium | 4.1 mmol/L |
| Serum chlorine | 110.0 mmol/L |
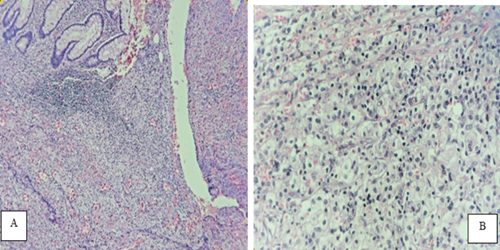
Figure 3 Histopathological report: Diagnosos of xanthogranulomatous appendicitis according to the cellular characteristics found and described below. A) Appendicular mucosa with abundant chronic and acute inflammatory infiltrate with transmural trac bordered by granulation and inflammatory tissue where there are abundant foamy histiocytes in the muscularis propria and subserosal(Hematoxylin-eosin,10X).B) Histiocytes with abundant foamy cytoplasm(Hematoxylin-eosin,40X)
DISCUSSION
XGI is a chronic inflammatory process that leads to local destruction of the tissues of the affected organ or those located in its vicinity. This type of inflammation has been described in kidney, gallbladder, prostate, epididymis, ovary and rarely in the cecal appendix. Histologically it has macrophages in which lipids are deposited with lymphocytes that give it a "foamy" appearance, plasma cells, neutrophils and cells. In this case, the histopathological study reported macroscopically perforated appendix in the middle third and tip, with fibrinous-purulent adhesions and thickened wall with subserous light yellow fociFigure 2.

Figure 2 Transverse section of the cecal appendix with transmural thickening showing light yellow foci
Proposed theories of the etiopathogenesis of this entity include abnormal lipid transport, immunological disorders of leukocyte and macrophage chemotaxis, infection by Proteus and Escherichia species that are of low virulence or by obstruction at the lymphatic level. However, in a study by Cozzuto et al. found that the xanthogranulomatous process is mainly associated with inflammation, hemorrhage and necrosis.3-5.
It has also been frequently observed in interval appendicitis, suggesting that late appendectomy often has a granulomatous inflammatory pattern with fibrosis, mural thickening and chronic transmural inflammation.4,5.
Its clinical presentation usually presents with pain in the right lower quadrant of the abdomen, fever, nausea and vomiting; other authors associate prolonged inflammation of the appendix with the formation of an appendiceal mass. Pathologies affecting the appendix catalogued in the atypical spectrum can simulate and cause a typical picture of acute appendicitis3.
Sometimes it is not possible to differentiate XGI from an infiltrative cancer because it may present as a tumor-like lesion with an extension of fibrosis and inflammation into the surrounding tissues6. Other inflammatory processes that cause granulomatous lesions and contain foam cells should be distinguished from XGI are Crohn's disease which is distinguished by the presence of transmural granulomas, and malakoplakia which is characterized by an inflammatory and destructive xanthomatous proliferation with the presence of Michaelis-Gutmann bodies or calcospherites (intracytoplasmic inclusion in concentric layers). Small localized xanthoma deposits without parenchymal destruction or xanthomas with prominent foam cell features found in tuberculous appendicitis should also be considered in the differential diagnosis3,6,7.
Another entity to rule out due to the chronicity of symptoms and the presence of a mass in the abdominal region is Spiegel's hernia, in which the appendix is rarely contained. Imaging studies are useful for diagnosis8; However, with exploratory laparotomy it could be ruled out when purulent liquid was obtained in the area where it was believed to be a hernia, a plastron was observed in the cecum and the cecal appendix was inflamed.
It is concluded from this case report that XGI does not have a specific clinical picture, the definitive diagnosis is obtained when the appendix is analyzed histologically and the treatment is surgical supplemented with broad-spectrum antibiotics.
REFERENCES
1. Lal DPCKA, Samarasekara N, Sivaganesh S, Zoysa I de. What Can Histopathology Say About Acute Appendicitis? Am J Clin Pathol. 2014;142:A233-A233. DOI:10.1093/ajcp/142.suppl1.233 [ Links ]
2. Kaushik R, Gulati A, Vedant D, Kaushal V. Cytological diagnosis of xanthogranulomatous appendicitis. J Cytol. 2017;34(1):48-50. doi: 10.4103/0970-9371.197619 [ Links ]
3. Akbulut S, Demyati K, Koc C, Tuncer A, Sahin E, Ozcan M, et al. Xanthogranulomatous appendicitis: A comprehensive literature review. World J Gastrointest Surg. 2021;13(1):76-86. DOI: 10.4240/wjgs.v13.i1.76 [ Links ]
4. Che Jusoh A, Abdul Ghani S. Xanthogranulomatous lesion in recurrent appendicitis. Formosan Journal of Surgery. 2016;49(3):114-118. Disponible en: https://doi.org/10.1016/j.fjs.2016.01.001 [ Links ]
5. Al-Rawabdeh SM, Prasad V, King DR, Kahwash SB. Xanthogranulomatous Appendicitis in a Child: Report of a Case and Review of the Literature. Case Rep Med. 2013:1-3. DOI: 10.1155/2013/498191 [ Links ]
6. Singh V, John KM, Malik A, Pareek T, Dutta V. Xanthogranulomatous appendicitis: Uncommon histological variant of a common entity. Med J Armed Forces India. 2015;71:S19-S21. DOI: 10.1016/j.mjafi.2012.11.003 [ Links ]
7. Ito S, Takahashi Y, Yamada T, Kawai Y, Ohira K. Xanthogranulomatous appendicitis with elevated tumor marker misdiagnosed as cecal cancer: a case report. J Surg Case Rep. 2021;2021(7):1-4. Disponible en: https://doi.org/10.1093/jscr/rjab274 [ Links ]
8. Martín-Mattar A, Isarraraz-Flores R, Ávila JP. Hernia de Spiegel y apendicitis aguda necrosada. Un reporte de caso. Cir Cir. 2020;88(6):782-786. Disponible en: https://doi.org/10.24875/ciru.20001112 [ Links ]
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: August 27, 2022; Accepted: September 18, 2022











 text in
text in