Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.23 no.1 Lima ene./mar. 2023 Epub 25-Ene-2023
http://dx.doi.org/10.25176/rfmh.v23i1.5309
Case Report
Gastrointestinal stromal tumor (GIST) in jejunum
1Facultad de Medicina de la Universidad Nacional de Trujillo, Trujillo, Peru.
Gastrointestinal stromal tumors (GIST) are mesenchymal neoplasms that represent less than 3% of gastrointestinal neoplasms, with an incidence of 1 to 2 cases per hundred thousand inhabitants. It originates more frequently in the stomach and small intestine and is characterized by the expression of the tyrosine kinase growth factor receptor, cd117. Therefore, its diagnosis requires an immunohischemical study to rule it out from other mesenchymal tumors. However, enteroscopic imaging and analysis of the biopsy may suggest a preoperative diagnosis of probable gist. The case of a 62-year-old woman with rectorrhagia and recurrent anemia caused by mid-intestinal bleeding observed by capsule endoscopy is reported. Enteroscopy revealed a subepithelial ulcerated lesion in the proximal jejunum, and a biopsy was taken, the anatomopathological study of which suggested a gastrointestinal stromal tumor. The biopsy sample subjected to immunohistochemical studies confirms the suspicion of a cKit/CD117-positive gist tumor. Surgical resection of the tumor with dimensions 4.2x3 cm is performed. After surgery, the patient was stable and under clinical follow-up until she was discharged. Clinical findings, diagnosis and timely treatment contribute to increasing survival from complications.
Keywords: gastrointestinal stromal tumor; cKit/CD117; midgastrointestinal hemorrhage. (source: mesh nlm).
Introduction
Gastrointestinal stromal tumors (GIST) are sarcomas that originate in the interstitial cells of cajal1; which are located within the muscle layer and are pacemaker cells of the gastrointestinal tract responsible for its motility2.
They are mostly caused by oncogenic mutations in the receptor tyrosine kinase (KIT gene) and smaller fractions have mutations in the platelet derived growth factor receptor alpha (PDGFRA) gene3, which encode members of the family of type iii transmembrane receptor tyrosine kinases, central regulators of cell proliferation, differentiation and apoptosis pathways1.
GISTS are rare and represent 1% to 2% of neoplasias. Gastrointestinal4. They can occur anywhere in the tract gastrointestinal5; however, they are more frequent in the stomach (51%), followed by the small intestine (36%), the colon (7%), the rectum (5%) and the esophagus (1%)2. It has a incidence of one to two per 100,000 individuals and a prevalence of 13 per 100,000 individuals, of which which men and women are equally affected5. These tumors can arise at any age and are most common in people between the ages of 40 and 70, with a median age of 65 years4,6.
Case report
It should be noted that the patient gave his informed consent for the report's publication. The article has been reviewed by the ethics committee and institutional permission for publication by the Hospital Regional Docente de Trujillo (HRDT).
A 62-year-old female patient from Magdalena de Cao, with a history of hospitalization at the Hospital Regional Docente de Trujillo (HRDT) from september 10 to 24, 2022, due to fainting, rectal bleeding (twice), hematemesis (three occasions) and abdominal swelling causing acute post-hemorrhagic anemia. Two globular packages were administered. An upper digestive endoscopy was performed, which failed to show evidence of a lesion causing bleeding in the esophagus, stomach, and duodenum. The colonoscopy showed the mucosa of the cecum and rectum conversed without evidence of lesions, and a CT scan revealed a solid nodule with uptake of the substance. Of contrast of exophytic growth in the jejunal wall, which suggests ruling out a gist tumor. (Figure 1)
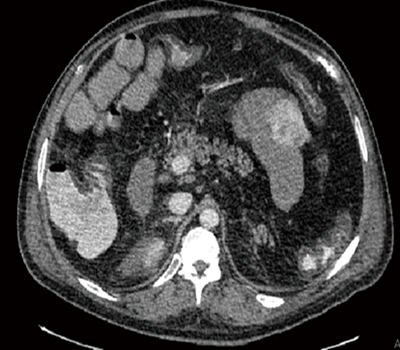
Figure 1 Computed axial tomography (CT) scan shows a 4.2 cm × 3.0 cm mass that enhanced heterogeneously within the proximal aspect of the jejunum about 15 cm from the treitz ligament
Likewise, an endoscopic capsule examination was performed, finding a lesion with an ulcerous impression and a subepithelial appearance. The HRDT did not have the capacity to perform an enteroscopy that could obtain a biopsy to rule out gist tumor. (Figure 2)
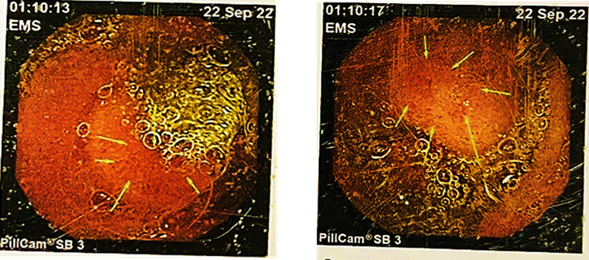
Figure 2 Capsule endoscopic examination where ulcerative impression lesions and subepithelial appearance are observed at time 01:10 of the procedure
The recommendations and treatment for discharge were a soft diet and control by an external gastroenterology clinic in 2 weeks.
On october 2, the patient went to the HRDT emergency department due to transrectal bleeding of approximately 500cc, vinous red in color and with foul-smelling clots with an evolution time of one day. She was referred to the gastroenterology service for observation and evaluation. On the day of admission, a globular package was administered, giving treatment with omeprazole (40 mg iv every 12 hours for 5 days), dimenhydrinate (50 mg iv pro re nata for 5 days) and tramadol (100 mg via EVpro re natafor 5 days). Two days after the date of admission, he presented 8.9g of hemoglobin and 27.2% of hematocrit. Four days later, his hemoglobin was 11.5% and his hematocrit was 35%; therefore, he was discharged with the diagnosis of inactive midgut bleeding with soft diet treatment, 20cc lactulose orally every 24 hours and referral to Chiclayo for his enteroscopy.
On october 14, an enteroscopy was performed at the Lambayeque regional hospital where an ulcerated subepithelial lesion of approximately 3cm in diameter was found with deep ulceration at its apex whose bed presented fibrin and remains of necrosis in the proximal jejunum. A biopsy is taken and surgical treatment is suggested.
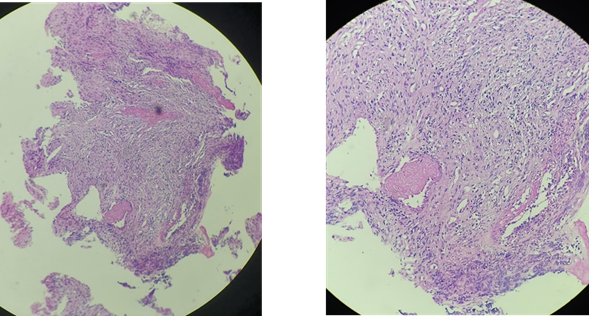
In the anatomopathological study, a spindle cell neoplasm suggestive of a gist tumor was diagnosed and an immunohistochemical study was indicated to define the lineage of the proliferating cells. (Figure 3)
For the surgery, she was referred to the Instituto Regional de Enfermedades Neoplásicas Norte (IREN norte) and was admitted as an emergency on november 2 for presenting her 4th rectal bleeding of approximately 250cc. In total, the patient received 7 red blood cells since the onset of the disease.
On november 6, resection of the jejunal gist tumor was performed. Among the operative findings, a tumor was found 15 cm from the angle of Treitz, a 4x3cm proliferative, extraluminal lesion that compromised 50% of the circumference of the intestinal wall of the first jejunal loop, for which we proceeded with the resection of 4 cm of intestine.
After the surgical procedure, the patient is stable and is hospitalized for follow-up until she is discharged.
The immunohistochemical result of the sample showed a positive gastrointestinal stromal tumor (GIST) for cKit/CD117. (mitotic rate <5 /5 mm). Spindle cells arranged in fascicles of intermediate cellularity with sectors of necrotic and hemorrhagic tissue, moderate-risk lesion with a size of 4.2 cm.
Discussion
GISTS are the most frequent mesenchymal neoplasms of the gastrointestinal tract, representing 0.1 to 3% of digestive tumors. Its incidence varies from 1 to 1.5 cases per 100,000 subjects per year; their age of presentation belongs to the range of 50 to 65 years and they are located in the hollow digestive viscera (80%) and in the retro-peritoneum and minor pelvis (10%)7,9. In addition, they originate in the interstitial cells of cajal of the intestinal nerve centers (myenteric plexus) by an activating mutation of the KIT (60-85%) and PDGF (10-15%) tyrosine kinase receptors10.
In this case report, the patient is a 62-year-old woman who suffers from digestive hemorrhage in the midgut, in addition to partial obstruction and chronic bleeding. It should be noted that approximately 70% of gist cases are symptomatic at diagnosis, but there is a small percentage that requires emergency surgery as in this case8. Likewise, the manifestations depend on three parameters, their location, aggressiveness and size. Tumors smaller than 2 cm are usually asymptomatic, limited to the colonic wall, and visible at endoscopy as small submucosal masses11. Among the operative findings of the case, a tumor was found 15 cm from the angle of treitz, a 4x3 cm extraluminal proliferative lesion that compromised 50% of the circumference of the intestinal wall of the first jejunal loop.
The most common complication of large GISTS is gastrointestinal bleeding secondary to mucosal ulceration, as occurred in this case, the main reason for the patient's consultation being rectal bleeding caused by the pelvic mass. Because GISTS range from benign to highly aggressive, risk stratification schemes based on prognostic factors such as size, site of origin, mitotic count, and proliferation index have been proposed12. Also, the diagnosis of bleeding jejunal GISTS is challenging due to their inaccessibility by endoscopy; for this reason, the immunohistochemical analysis of the samples was chosen, where they expressed cd117 (95%), cd34 (60-70%) and smooth muscle actin alpha (20-40%), as well as positive vimentin and negative desmin to differentiate them. Of melanomas and plasmacytomas13. And, given the finding of nonspecific abdominal pain and other nonspecific gastrointestinal signs and symptoms, gastrointestinal bleeding, resistance to treatment, and coexistence of an abdominopelvic mass, this type of tumor should be considered in the differential diagnosis. Timely diagnosis and treatment will help improve the patient's chances of survival.
Acknowledgments
To doctors calvo arana héctor, requena fuentes víctor raúl and diaz plasencia juan alberto, for giving us their valuable support and collaboration in the development of this research work.
REFERENCES
1. Akahoshi k, oya m, koga t, shiratsuchi y. Current clinical management of gastrointestinal stromal tumor. World j gastroenterol. 2018;24(26):2806-17. Disponible en: https://doi.org/10.3748/wjg.v24.i26.2806 [ Links ]
2. Blay jy, kang yk, nishida t, von mehren m. Gastrointestinal stromal tumours. Nat rev dis primer. 2021;7(1):1-22. Disponible en: https://doi.org/10.1038/s41572-021-00254-5 [ Links ]
3. Al-share b, alloghbi a, al hallak mn, uddin h, azmi a, mohammad rm, et al. Gastrointestinal stromal tumor: a review of current and emerging therapies. Cancer metastasis rev. 2021;40(2):625-41. Disponible en: https://doi.org/10.1007/s10555-021-09961-7 [ Links ]
4. Parab tm, derogatis mj, boaz am, grasso sa, issack ps, duarte da, et al. Gastrointestinal stromal tumors: a comprehensive review. J gastrointest oncol. 2019;10(1):144-54. Disponible en: https://doi.org/10.21037/jgo.2018.08.20 [ Links ]
5. Mantese g. Gastrointestinal stromal tumor: epidemiology, diagnosis, and treatment. Curr opin gastroenterol. 2019;35(6):555-9. Disponible en: https://doi.org/10.1097/mog.0000000000000584 [ Links ]
6. Sorour ma, kassem mi, ghazal aeha, el-riwini mt, abu nasr a. Gastrointestinal stromal tumors (gist) related emergencies. Int j surg. 2014;12(4):269-80. Disponible en: https://doi.org/10.1016/j.ijsu.2014.02.004 [ Links ]
7. Saad mk, hajj ie, saikaly e. Jejunal gastrointestinal stromal tumor (gist): a case report presenting as life threatening emergency. Gastrointest stromal tumor [internet]. El 20 de noviembre de 2020 [citado el 23 de noviembre de 2022];3(0). Disponible en: https://doi.org/10.1016/j.ijsu.2014.02.004 [ Links ]
8. Gom169j.pdf [internet]. [citado el 23 de noviembre de 2022]. Disponible en: https://www.medigraphic.com/pdfs/ginobsmex/gom-2016/gom169j.pdf [ Links ]
9. Pinilla-lizarraga r, claros-beltrán n, mayte-arze g. Neoplasia fusocelular - tumor de gist: presentación de un caso. Cuad hosp clínicas. Diciembre de 2020;61(2):51-7. Disponible en: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1179195 [ Links ]
10. Moreno-paquentín e, caba molina d, sánchez-garcía j, arrangoiz-majul r, cordera-gonzález de cosío f, luque de león e, et al. Reporte de caso clínico de un tumor del estroma gastrointestinal (gist) gigante y revisión bibliográfica. Cir gen. Junio de 2018;40(2):127-32. Disponible en: https://www.medigraphic.com/pdfs/cirgen/cg-2018/cg182j.pdf [ Links ]
11. Sashidharan p, matele a, matele u, al felahi n, kassem kf. Gastrointestinal stromal tumors: a case report. Oman med j. Marzo de 2014;29(2):138-41. Disponible en: https://doi.org/10.5001/omj.2014.34 [ Links ]
12. Joensuu h, wardelmann e, sihto h, eriksson m, sundby hall k, reichardt a, et al. Effect of kit and pdgfra mutations on survival in patients with gastrointestinal stromal tumors treated with adjuvant imatinib: an exploratory analysis of a randomized clinical trial. Jama oncol. El 1 de mayo de 2017;3(5):602-9. Disponible en: https://doi.org/10.1001/jamaoncol.2016.5751 [ Links ]
13. Soriano-lorenzo j, lima-pérez m, soriano-garcía j, zaldívar-blanco k, fleites-calvo v. Tumores del estroma gastrointestinal. An fac med. Abril de 2019;80(2):214-21. Disponible en: https://doi.org/10.15381/anales.802.16418 [ Links ]
8 Article published by the journal of the faculty of human medicine of the ricardo palma university. It is an open access article, distributed under the terms of the creatvie commons license: creative commons attribution 4.0 international, cc by 4.0(https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: December 09, 2022; Accepted: January 12, 2023











 texto en
texto en