Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.23 no.2 Lima abr./jun. 2023 Epub 18-Abr-2023
http://dx.doi.org/10.25176/rfmh.v23i2.5642
Original Article
Quality of life with and without sphincter-conserving surgery for real cancer
1Instituto Mexicano Del Seguro Social, Centro Médico Nacional, Hospital De Especialidades “Gral. Div. Manuel Ávila Camacho”, Departamento De Cirugía Digestiva. Puebla, Mexico.
2Instituto Mexicano Del Seguro Social, Centro Médico Nacional, Hospital De Especialidades “Gral. Div. Manuel Ávila Camacho”, Dirección De Educación E Investigación En Salud. Puebla, Mexico.
3Faculty Of Medicine, Universidad Popular Autónoma Del Estado De Puebla, Puebla De Zaragoza, Mexico.
Introduction:
Colorectal cancer (CRC) is the third most common cancer and the second leading cause of death worldwide, with an incidence of 10.2%. The treatment of CRC has evolved over the past 25 years. Two surgical procedures are used: abdominoperineal resection (APR) and low anterior resection (LAR) and ultra-low anterior resection (ULAR). The recurrence rate and quality of life are similar between these approaches.
Objective:
To compare the quality of life of rectal cancer patients treated with abdominoperineal resection versus conservative sphincter-preserving surgeries: low anterior resection (LAR) and ultra-low anterior resection (ULAR) at UMAE of Puebla.
Methods:
A comparative, observational, cross-sectional study was conducted on CRC patients treated between 2015 and 2019 at a tertiary-level hospital in Puebla. Two groups were formed: those managed with APR and those managed with LAR/ULAR. The EORTC QLQ-CR29 scale and EuroQol were applied. Descriptive statistics and the Mann-Whitney U test were used for comparisons.
Results:
A total of 26 patients were recruited, 18 with APR and 8 with LAR/ULAR. The mean quality of life score in the APR group was 73.72 (SD 16.92, minimum 31.46, maximum 95.09), and in the LAR/ULAR group was 56.22 (SD 6.29, minimum 47.51, maximum 68.96), with a p-value of 0.005.
Conclusions:
There is no significant difference in the quality of life of CRC patients operated with APR, LAR, and ULAR (non-conservative and conservative approaches).
Keywords: Neoplasm; quality of life; anastomosis; surgical. (Source: MeSH - NLM).
INTRODUCTION
Colorectal cancer (CRC) is the third most common cancer and the second leading cause of death worldwide, with an incidence of 10.2%1,2. The five-year survival rate in high-income countries in 2020 ranged from 59% to 70.9% of the affected population3,4.
While the most common presentation occurs in individuals over 70 years old, the incidence among individuals under 50 years old has increased up to 1.8% per year5. This increase affects the productive population of the country and the life expectancy of 75 years6,7.
The anatomy of the rectum poses a challenge for surgeons: inadequate dissection from the midline towards the endopelvic fascia can lead to local recurrence of the disease. Improper avascular lateral dissection compromises autonomic nerves and causes impotence in men, general bladder dysfunction, as well as intestinal motility disorders and body image disturbances.8,9.
The treatment of CRC has changed over the past 25 years10. The goal of colorectal surgery is to maintain clear margins free from malignancy8.
Multimodal therapy and surgery with clear margins have shown low rates of local recurrence and improved long-term survival11,12.
Two surgical approaches are used: abdominoperineal resection (APR) involves complete anorectal removal, with permanent residual colostomy and no preservation of anal sphincters13. In contrast, low anterior resection and ultra-low anterior resection (LAR/ULAR) involve colorectal anastomosis and sphincter preservation14,15.
The presence of permanent stomas decreases the quality of life (QoL) for patients managed with APR15. On the other hand, patients undergoing LAR/ULAR have a risk of developing low anterior resection syndrome, which significantly affects the patient's long-term QoL16,17.
The indications for sphincter-preserving surgery have increased in order to avoid a permanent stoma18. These patients experience intestinal symptoms such as incomplete evacuation, loose stools, and/or gas incontinence after surgery, which also diminishes their QoL19,20.
However, recent reports indicate similar rates of recurrence and QoL between sphincter-conserving surgery and APR18,19.
All of this represents a dilemma in choosing the surgical approach20.
Inter-sphincteric resections and reduced distal margins are currently areas of exploration but with limited technological availability21,22.
The high incidence of complications is due to extensive resection, leaving the pelvic cavity exposed to infections23,24.
The objective of this study was to compare the QoL in patients with CRC managed with APR versus those with sphincter preservation (LAR/ULAR) at a tertiary-level hospital of the Instituto Mexicano del Seguro Social.
METHODS
Design and study area
A comparative, prospective and retrospective, cross-sectional study was conducted on patients treated at a tertiary-level hospital of the Instituto Mexicano del Seguro Social in Puebla, Mexico, during 2015-2019.
Population and sample
Using non-probabilistic convenience sampling, 26 medical records of 47 patients who underwent surgery for CRC with APR or LAR/ULAR and met the inclusion criteria were included. Those who passed away, discontinued follow-up through outpatient visits, or did not answer the phone call were excluded.
APR was considered for cases with complete rectal resection in tumors located five cm below the anal margin, using abdominal and perineal approaches, with permanent residual colostomy and no preservation of anal sphincters.
Sphincter-preserving surgeries included LAR/ULAR for tumors located up to six and two cm from the anal margin, respectively, performed through laparotomy. Both procedures involved colorectal mechanical anastomosis with or without a protective stoma.
Variables and instruments
Age and gender of CRC patients were recorded.
The “European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire - Colorectal Cancer Module 29” (EORTC QLQ-CR29) was administered. It consists of four functional scales (body image, sexual function, sexual enjoyment, future perspectives) and seven symptom scales (urinary problems, gastrointestinal problems, chemotherapy side effects, sexual dysfunction, defecation problems, weight loss, stoma-related problems).
The EuroQol questionnaire, consisting of five dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression), each with three levels (no problems, some problems or moderate problems, and severe problems), was also administered22,24.
The scores from the application of the EORTC QLQ-CR29 were stratified as follows: 100-67.85 = good quality of life and 67.84-35.711 = poor quality of life. For EuroQol, a score of 1-0.757 was considered good quality of life and 0.756-0.0514 was considered poor quality of life24.
Procedures
The required information was collected from the patients' records who met the selection criteria.
After obtaining informed consent in the outpatient clinic, the EORT QLQ CR-29 and EuroQol questionnaires were administered to the patients.
RESULTS
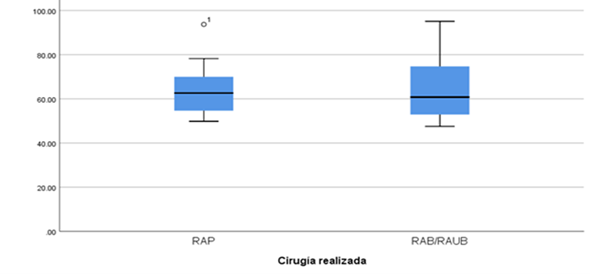
26 out of a total of 47 patients were surveyed; 18 could not be contacted (did not answer the phone and/or changed address without traceability), two passed away, and one declined to participate in the study. The gender distribution was 14 females (54%) and 12 males (46%). The mean age was 61.76 years (standard deviation (SD) 11.99, minimum 35, maximum 82). Eight (30.8%) patients reported having diabetes mellitus, six (23.1%) had hypertension, and one patient (3.8%) had other respiratory, cardiac, rheumatological, and inflammatory bowel diseases in each entity. Patients who underwent APR had a mean QoL of 73.72 (SD 16.92, minimum 31.46, maximum 95.09). Those with LAR/ULAR had a mean of 56.2 (SD 6.29, minimum 47.51, maximum 95.09). The Mann-Whitney U test yielded a p-value of 0.952 (95% CI). SeeFigure 1
Abbreviations: APR: abdominoperineal resection, LAR: low anterior resection, ULAR: ultralow anterior resection. EORTC QLQ-C29 application score: good: 100-67.85, bad: 67.84-35.71.
The Shapiro-Wilk test was applied to all variables, resulting in a p-value <0.05. When comparing the quality of life between patients treated with APR and LAR/ULAR, no significant differences were found. The details are shown inTable 1
Table 1. Quality of life according to symptoms.
| Non-Conservative APR | Conservative LAR/ULAR | Difference in medians | U | P | |||||
| Body image | Med | 0.79 | 0.95 | 0.16 | 61.50 | 0.553 | |||
| Min | 0.5 | 0.41 | |||||||
| Max | 1 | 1 | |||||||
| Sexual health | Med | 0.15 | 0.12 | 0.03 | 67.00 | 0.762 | |||
| Min | 0.12 | 0.12 | |||||||
| Max | 0.81 | 1 | |||||||
| Urinary symptoms | Med | 0.87 | 0.91 | 0.04 | 69.00 | 0.865 | |||
| Min | 0.58 | 0.74 | |||||||
| Max | 1 | 1 | |||||||
| Gastrointestinal symptoms | Med | 0.90 | 0.95 | 0.05 | 51.00 | 0.230 | |||
| Min | 0.25 | 0.64 | |||||||
| Max | 1 | 1.66 | |||||||
| Chemotherapy symptoms | Med | 0.99 | 0.95 | 0.04 | 45.50 | 0.119 | |||
| Min | 0.33 | 0.49 | |||||||
| Max | 1 | 1 | |||||||
| Health concern in the future | Med | 0.50 | 0.75 | 0.25 | 60.00 | 0.484 | |||
| Min | 0.25 | 0.25 | |||||||
| Max | 1 | 1 | |||||||
Med: Median. Min: Minimum. Max: Maximum. APR: Abdominoperineal resection. LAR: Low anterior resection. ULAR: Ultra-low anterior resection.
DISCUSSION
Colorectal cancer is a common cancer with high mortality rates. Surgery remains a fundamental part of CRC treatment. The management involves multimodal therapy with low recurrence rates; however, these treatments impact the patient's quality of life10,25. This study compares the quality of life of CRC patients treated with APR versus sphincter-preserving resections: LAR and ULAR.
CRC ranks third in terms of incidence, with a reported incidence of 10.9% in males and 9.5% in females1,26. This study found a slight predominance of females, accounting for 54% of the patients.
Patients undergoing APR in this study had a mean quality of life score of 73.72 (good quality of life). They reported urinary and gastrointestinal symptoms, as well as body perception and sexuality, without interference in their quality of life. Some studies have reported better quality of life in patients undergoing APR, while others have concluded that there are no differences in quality of life based on the type of intervention27,28.
Patients undergoing LAR/ULAR in this study had a score of 56.22 (poor quality of life). They reported that their sexual health affected their quality of life, while urinary, gastrointestinal, and body perception symptoms did not interfere with it. Patients undergoing LAR/ULAR did not report urinary symptoms, sexual problems, or body perception issues27.
APR interventions are more frequently associated with postoperative complications, perianal infections, and delayed wound healing29. A higher local recurrence rate and a 5-year survival rate were observed in APR. The one-year comparison of quality of life in patients with APR versus LAR/ULAR was lower in APR30.
Studies have concluded that there are no differences in age, sex, education, cancer duration, and stage among patients undergoing APR compared to LAR/ULAR31,32. Both procedures were evaluated to improve psychological and emotional well-being, although patients undergoing LAR/ULAR stood out for their notable progress33.
CONCLUSION
There is no significant difference in the quality of life of CRC patients operated on with APR, LAR, and ULAR (conservative and non-conservative approaches).
Patient counseling is recommended before performing APR or LAR/ULAR34, as the decision is based on the information provided by the patient and whether they are willing to tolerate more intestinal symptoms to avoid a permanent colostomy35.
REFERENCES
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68(6):394-424. doi: 10.3322/caac.21492 [ Links ]
2. Downing A, Morris EJ, Richards M, Corner J, Wright P, Sebag-Montefiore D, et al. Health-related quality of life after colorectal cancer in England: A patient-reported outcomes study of individuals 12 to 36 months after diagnosis. J Clin Oncol 2015;33(6):616-24. doi: 10.1200/JCO.2014.56.6539 [ Links ]
3. Keller DS, Berho M, Perez RO, Wexner SD, Chand M. The multidisciplinary management of rectal cancer. Nat Rev Gastroenterol Hepatol. 2020 Jul;17(7):414-429. doi: 10.1038/s41575-020-0275-y [ Links ]
4. Burbano-Luna DF, Antonio-Manrique M, Chávez-García MA, Pérez-Corona T, Hernánde- Velázquez NN, Escandón-Espinoza YM, et al. Epidemiología del cáncer colorrectal en menores de 50 años en el Hospital Juárez de México. Endoscopia 2016;28(4):160-165. doi: 10.1016/j.endomx.2016.10.008 [ Links ]
5. INEGI. Esperanza de vida al nacimiento por entidad federativa según sexo, serie anual de 2010 a 2021. Disponible en: https://www.inegi.org.mx/app/tabulados/interactivos/?pxq=Mortalidad_Mortalidad_09_61312f04-e039-4659-8095-0ce2cd284415 [ Links ]
6. INEGI. Esperanza de vida al nacimiento por entidad federativa según sexo, serie anual de 2010 a 2021. Disponible en: https://www.inegi.org.mx/app/tabulados/interactivos/?pxq=Mortalidad_Mortalidad_09_61312f04-e039-4659-8095-0ce2cd284415 [ Links ]
7. CONAPO. Consejo Nacional de Población. Datos Abiertos. Indicadores demográficos 1950 - 2050. (Consulta: 11 de enero de 2022). Disponible en: https://datos.gob.mx/busca/dataset/proyecciones-de-la-poblacion-de-mexico-y-de-las-entidades-federativas-2016-2050 [ Links ]
8. Mahmoud NN, Bleiber JIS, Aarons CR, Paulson EC, Shanmungan S, Fry RD. Colon and Rectum. En: Courtney M. Townsend, Jr, R. Daniel Beauchamp, B. Mark Evers, Kenneth L. Mattox. Sabiston textbook of surgery: the biological basis of modern surgical practice. 20th edición. Huston, Texas: Elsevier; 2017. 1312-91. Disponible en: https://handoutset.com/wp-content/uploads/2022/06/Sabiston-Textbook-of-Surgery-Townsend-C.M.-Beauchamp-R.D.-Evers-etc..pdf [ Links ]
9. Wilkinson N. Management of Rectal Cancer. Surg Clin North Am 2020;100(3):615-628. doi: 10.1016/j.suc.2020.02.014 [ Links ]
10. Hendren S, Abdelsattar Z. Sphincter-Preserving Surgery for Rectal Cancer: A Controversial Measure of Quality. Ann Surg Oncol 2015;22:9-10. doi: 10.1245/s10434-014-4104-9 [ Links ]
11. Carrillo-G K, Abedrapo-M M, Azolas-M R. Técnicas quirúrgicas para la preservación de esfínter en cáncer de recto bajo: revisión histórica y estado actual. Rev Chil Cir. 2018;70(2):178-84. doi: 10.4067/s0718-40262018000200178 [ Links ]
12. Fischer, A., Tarantino, I., Warschkow, R., Lange, J., Zerz, A., & Hetzer, F. H. (2010). Is sphincter preservation reasonable in all patients with rectal cancer? Int J Colorrectal Dis, 25(4), 425-432. doi: 10.1007/s00384-010-0876-y [ Links ]
13. Annicchiarico A, Martellucci J, Solari S, Scheiterle M, Bergamini C, Prosperi P. Low anterior resection syndrome: can it be prevented? International Journal of Colorectal Disease. 2021: 1-18. doi: 10.1007/s00384-021-04008-3 [ Links ]
14. Fokas E, Glynne-Jones R, Appelt A, Beets-Tan R, Beets G, Haustermans K, et al. Outcome measures in multimodal rectal cancer trials. Lancet Oncol 2020;21(15):e252-64. doi: 10.1016/S1470-2045(20)30024-3 [ Links ]
15. Espín E, Armengol M. Radioterapia en el cáncer de recto. Estado actual. Cir Esp 2004;76(6):347-52. doi: 10.1016/S0009-739X(04)72393-3 [ Links ]
16. Valverde A. Cirugía del cáncer rectal por laparotomía y laparoscopia. EMC - Técnicas Quirúrgicas - Apar Dig 2019;35:1-30. doi: 10.1016/s1282-9129(19)42465-3 [ Links ]
17. Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL. Anterior resection syndrome. Lancet Oncol 2012;13(9):e403-8. doi: 10.1016/S1470-2045(12)70236-X [ Links ]
18. Lynes KV. Determinants of sphincter preservation in low rectal surgery for cancer [tesis doctoral]. London: Queen Mary, University of London; 2020. Disponible en: https://qmro.qmul.ac.uk/xmlui/handle/123456789/69452 [ Links ]
19. Park J, Neuman HB, Bennett AV, Polskin L, Phang PT, Wong WD, et al. Patients' Expectations of Functional Outcomes Following Rectal Cancer Surgery: a Qualitative Study. Dis Colon Rectum. 2022; 57(2): 151-157. doi: 10.1097/DCR.0000000000000036 [ Links ]
20. Chen TY-T, Emmertsen KJ, Laurberg S. Bowel dysfunction after rectal cancer treatment: a study comparing the specialist's versus patient's perspective. BMJ Open. 2013; 4: e003374. doi: 10.1136/bmjopen-2013-003374 [ Links ]
21. Whistance RN, Conroy T, Chie W, Costantini A, Sezer O, Koller M, et al. European Organisation for the Research and Treatment of Cancer Quality of Life Group. Clinical and psychometric validation of the EORTC QLQ-CR29 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer. 2009 Nov;45(17):3017-26. doi: 10.1016/j.ejca.2009.08.014 [ Links ]
22. Calvo Ó, Oliveros R, Sánchez R. Adaptación cultural del formulario EORTC QLQ CR-29 para su aplicación en pacientes con cáncer de recto en el Instituto Nacional de Cancerología de Colombia. Rev Colomb Cancerol 2010;14(4):189-98. doi: 10.1016/s0123-9015(10)70082-2 [ Links ]
23. Cádernas de la Maza R, Pizarro-Núñez P. Resección abdominoperineal del recto, Análisis de la morbimortalidad operatoria. Rev Chilena de Cirugía. 2002; 54(1): 21-26. Disponible en: https://www.cirujanosdechile.cl/revista_anteriores/PDF%20Cirujanos%202002_01/Cir.1_2002%20Resec.abdominoperine.pdf [ Links ]
24. Arraras JI, Vera R, Manterola A, Martínez M, Arias F, Martínez E, et al. El cuestionario de Calidad de Vida para cáncer colorectal EORTC QLQ-CR38. Estudio de validación para España. Oncología (Barc) 2003;26(9):285-92. Disponible en: https://pesquisa.bvsalud.org/portal/resource/pt/ibc-26391?lang=es [ Links ]
25. Moreno-B N, Bocic-A G, Carrillo-G K, López-N S, Abedrapo-M M, Sanguineti-M A, et al. Evaluación comparativa en calidad de vida de pacientes con RAUB, RAUBIE vs RAP por cáncer de recto. Informe preliminar. Rev Cir (Mex) 2019;71(1):22-28. doi: 10.4067/s2452-45492019000100022 [ Links ]
26. Herrera-Mostacero J, Diaz-Plasencia J, Fermín-Yan-Quiroz E. Comparación de la Percepción de la Calidad de Vida en pacientes con Tratamiento Quirúrgico y/o Adyuvante en Cáncer de Colon y Cáncer de Recto en el Instituto Regional de Enfermedades Neoplásicas (Trujilo). Rev Gastroenterol. Perú 2010;30(2):137-147. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292010000200006&lng=es [ Links ]
27. Kang SB, Cho JR, Jeong SY, Oh JW, Ahn S, Choi S. Quality of life after sphincter preservation surgery or abdominoperineal resection for low rectal cancer (ASPIRE): A long-term prospective, multicentre, cohort study. The Lancet Regional Health - Western Pacific. 2021; 6: 1-11. doi: 10.1016/j.lanwpc.2020.100087 [ Links ]
28. Dumont F, Goéré D, Honoré C, Elias D. Comparison of Fecal Continence and Quality of Life Between Intersphincteric Resection and Abdominoperineal Resection Plus Perineal Colostomy for Ultra-Low Rectal Cancer. Journal of Surgical Oncology. 2013; 108:225-229. doi: 10.1002/jso.23379 [ Links ]
29. Kose J, Tarantino I, Kulu Y, Bruckner T, Trefz S, Schmidt T. Sphincter-Preserving Surgery for Low Rectal Cancer: Do We Overshoot the Mark? J Gastrointest Surg. 2017; 21: 885-891. doi: 10.1007/s11605-016-3339-0 [ Links ]
30. Hawkins AT, Albutt K, Wise PE, Alavi K, Sudan R, Kaiser AM, Bordeianou L; Continuing Education Committee of the SSAT. Abdominoperineal Resection for Rectal Cancer in the Twenty-First Century: Indications, Techniques, and Outcomes. J Gastrointest Surg. 2018 Aug;22(8):1477-1487. doi: 10.1007/s11605-018-3750-9 [ Links ]
31. De Campos-Lobato LF, Alves-Ferreira PC, Lavery IC, Kiran RV. Abdominoperineal resection does not decrease quality of life in patients with low rectal cancer. Clinics. 2011; 66(6): 1035-1040. doi: 10.1590/S1807-59322011000600019 [ Links ]
32. Bossema E, Stiggelbout A, Baas-Thijssen M, van de Velde C, Marijnen C. Patients' preferences for low rectal cancer surgery. EJSO. 2008; 34(1): 42-48. doi: 10.1016/j.ejso.2007.08.007 [ Links ]
33. Cornish JA, Tilney HS, Heriot AG, Lavery IC, Fazio VW, Tekkis PP. A Meta-Analysis of Quality of Life for Abdominoperineal Excision of Rectum versus Anterior Resection for Rectal Cancer. Ann Surg Oncol. 2007 Jul;14(7):2056-68. doi: 10.1245/s10434-007-9402-z [ Links ]
34. Konanz J, Herrle F, Weiss C, Post S, Kienle P. Quality of life of patients after low anterior, intersphincteric, and abdominoperineal resection for rectal cancer-a matched-pair analysis. Int J Colorrectal Dis. 2013; 28: 679-688. doi: 10.1007/s00384-013-1683-z [ Links ]
35. Lee L, Trepanier M, Renaud J, Liberman S, Charlebois P, Stein B, Fried GM, Fiore J Jr, Feldman LS. Patients' preferences for sphincter preservation versus abdominoperineal resection for low rectal cancer. Surgery. 2021 Mar;169(3):623-628. doi: 10.1016/j.surg.2020.07.020 [ Links ]
8 Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: December 07, 2022; Accepted: April 13, 2023











 texto en
texto en