Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.23 no.2 Lima abr./jun. 2023 Epub 18-Abr-2023
http://dx.doi.org/10.25176/rfmh.v23i2.5582
Original Article
Factors associated with quality of life in older adults with advanced chronic organ failure in a hospital in Lima-Peru
1Universidad Nacional Mayor De San Marcos. School Of Medicine. Lima, Peru.
2Universidad Científica Del Sur. Lima, Peru.
3Caredoctors Foundation Training Unit. Faculty Of Medicine. International University Of Catalonia.
4Geriatrics Service, Centro Medico Naval, Callao, Peru.
Objective:
To determine the factors associated with the quality of life in older adults with advanced chronic organ failure in a hospital in Lima-Peru.
Materials and methods:
Observational research, cross-sectional analysis, whose population was made up of 100 older adults, the collection technique was the interview and the instrument the questionnaire through the application of the Barthel index and WHOQoL-Bref. To respond to the study objectives, the non-parametric Mann Whitney u, Kruskal Wallis and Spearman's Rho tests were applied, considering the significance of 5%.
Results:
(44) 44% of older adults were over 80 years old, (59) 59% were men, (31) 31% studied a higher technical level, (57) 57% were incumbents in the navy, (74) 74% had arterial hypertension. The most frequent geriatric syndromes were visual or auditory deficit (82) 82%, insomnia (59) 59%, constipation (52) 52% and malnutrition (47) 47%. The (50) 50% of the older adults presented severe functional dependence. (63) 63% presented quality of life at a medium level. The epidemiological factors associated with low quality of life were age over 80 years (p=0.032, RP=1.818), female sex (p=0.009, RP=2.056), the level of education given by illiterate, primary and secondary school (p=0.025, RP=1.930) and the relationship with the navy as a family member (p=0.022, RP=1.894). Associated geriatric syndromes were insomnia (p=0.034, RP=1.930), constipation (p=0.000, RP=3.560), pressure injury (p=0.000, RP=2.788) and severe functional dependence (p= 0.000, PR=4.667). However, the multivariate analysis showed that insomnia (p=0.002; RPa=1.166), pressure injury (p=0.016; RPa=1.248) and severe dependence (p=0.000; RPa=1.207) were the associated factors. Significantly to the low quality of life in older adults.
Conclusions:
The factors insomnia, pressure injury and severe dependency were significantly associated with low quality of life in older adults with advanced chronic organ failure in a hospital in Lima-Peru.
Keywords: associated factors; quality of life; older adults.
INTRODUCTION
Population aging is a demographic phenomenon of global reach1,2, which often presents a variety of challenges for healthcare systems, as it requires maximizing the health and functional capacity of older adults, as well as their safety and participation in society3,4, However, in this population, it is often identified that their needs and requirements are not being met5,6, This has led to the growth of chronicity, whose approach is based on three end-of-life trajectories: oncologic diseases, dementia - frailty, and chronic organ failure7.
Advanced chronic organ failure may affect 1% of the adult population, and it is assumed that 75% of patients with progression of one or more organ failures will have fatal outcomes.8, For this reason, it not only involves a gradual deterioration of health but also changes in habits and daily life, functional and nutritional limitations, impairment of socio-family life, constant dependence on clinical follow-up and even existential conflicts and spiritual anguish, aspects that have a direct impact on the patient's quality of life9,10.
Based on the quality of life, in Peru, in the year 2000, the "National Plan for Older Adults (PLANPAM)" was created, which promotes active and healthy aging through four national policies: "healthy aging", "employment, social security and social security", "participation and social integration" and "education, awareness and culture on aging and old age", thus encompassing human rights, gender equality and intergenerationality in older adults.11.
Given the above, the scientific community made it essential to investigate those characteristics or features of exposure associated with the quality of life of older adults with advanced chronic organ failure, highlighting among the main factors age over 75 years, male sex, low level of education, presence of more than 2 comorbidities, time of illness over 3 years, frailty, polypharmacy, functional dependence, and severe clinical manifestations.10,12,13.
However, these characteristics or features have been identified in international contexts, so considering that these are modifiable by the geographical distribution and public health policies of each country, it is necessary to conduct this research to establish evidence-based records for the evaluation of the needs of this population and respond to the most prevalent promptly, to increase the supply and intensity of care aimed at improving the quality of life, through scheduled care, accessibility of services, crisis prevention and emergency care. Therefore it must be taken into account to respond to the ethical challenges of promoting benefits and risk reduction, ensuring the exercise of patient rights; Therefore, the objective of this study was to establish the factors associated with quality of life in older adults with advanced chronic organ failure in a hospital in Lima-Peru.
MATERIALS AND METHODS
Design and study area
This study had an observational, cross-sectional analytical design.
The study was carried out at the "Cirujano Mayor Santiago Távara" Naval Medical Center, located at Av. Venezuela s/n, district of Bellavista, Lima-Callao-Peru. This center is a level III health care institution, which was inaugurated in 1956, by Supreme Resolution Nº153-1952. Its mission is based on providing quality health care to active Naval Personnel, as well as those in retirement and their families; while its vision is aimed at achieving sustainable care of excellence, directed by the Naval Personnel and entitled family members, with highly trained personnel and the latest technology.
Population and sample
The population consisted of 100 older adults attended at the "Cirujano Mayor Santiago Távara" Naval Medical Center between April and July 2021. Since the population was accessible, the entire population was considered as a sample. The technique and type of sampling applied were non-probabilistic and census 14. In addition, it was taken into consideration that the size of the sample allows for the corresponding statistical analysis for this type of study (minimum of 64 cases evaluated)15.
Patients aged 60 years or older, with advanced organ failure at cardiac, respiratory, renal and/or advanced cirrhosis level were included. Older adults with a diagnosis of cognitive impairment recorded in the clinical history with Mini-Mental State Examination (MMSE) less than 24 were excluded.
Severe and persistent clinical manifestations ((Functional Class III and IV New York Heart Association) are considered criteria for advanced heart failure(16), in addition to severe cardiac dysfunction (left ventricular ejection force less than or equal to 30%, congenital or valvular anomalies that do not qualify for intervention and severe diastolic dysfunction with increased natriuretic peptides)16.
Advanced respiratory failure is characterized by a forced expiratory volume in the first second (FEV1) less than 30% or less than 50% in relation to the reference value, with the presence of respiratory or right heart failure and forced vital capacity (FVC) less than 70%17.
On the other hand, advanced renal failure involves two specific stages: Stage IV: characterized by evidence of a glomerular filtration rate ranging between 15 and 29 ml/min/1.73 m2and stage V: characterized by evidence of a glomerular filtration rate lower than 15 milliliters/min/1.73 m218.
Finally, advanced chronic liver disease, also called decompensated cirrhosis, represents the late phase of gradual liver fibrosis and the compromise of liver structure and the configuration of regenerative nodules19.
Neuropsychiatric diseases recorded in the clinical history were considered as exclusion criteria. For dementia, the neuropsychological report and psychiatric conditions such as schizophrenia, bipolar disorder, and diagnoses established by the Mental Health specialty were considered.
Variables and instruments
The collection technique used was the structured interview and a questionnaire was used as an instrument.
The independent variables were age, sex, educational level, relationship to the Navy, comorbidity, time of advanced organ failure, geriatric syndromes such as visual or hearing impairment as assessed by patient self-report, insomnia assessed as difficulty falling asleep, constipation identified by the presence of hard stools, straining defecation, loose stools or frequency of bowel movements less than 3 times per week, malnutrition, presence of albumin value less than 3.5 mg/dl, falls assessed as the number of falls in the last 6 months, pressure injury defined by the presence of skin lesions of the skin less than 3.5 mg/dl, pressure injury defined by the presence of skin lesions of the skin less than 3 times per week, malnutrition, presence of albumin value less than 3.5 mg/dl, falls valued as the number of falls in the last 6 months, pressure injury defined by the presence of skin lesions produced by pressure against a surface and functional dependence, measured with the Barthel Index, which analyzes 10 aspects of the person's daily activity, by means of 30 items, where each one of them has scores from 0 to 10, with a total score of 100 points, the categories are: total dependence (0 to 20 points), severe (21 to 60 points), moderate (61 to 90 points), mild (91 to 99 points) and independent (100 points)20. which has a Cronbach's alpha of 0.90 to 0.9221.
The dependent variable will be the quality of life, quantified with the WHOQoL-Bref (22.
The other 24 are divided into 4 dimensions or areas: physical health, psychological health, social relations and environment. The scores range from 0 to 100, where 0 is equivalent to the worst quality of life and 100 to the best23. In addition, these scores also allow the quality of life to be categorized as low (0 to 59 points), medium (60 to 90 points) and high (91 to 120 points)24. This instrument has been validated in Chile (Cronbach's alpha = 0.94)22and the Colombian (Cronbach's Alpha = 0.80)25. For the present investigation a pilot test was carried out with the participation of 26 patients, finding a good reliability through the application of Cronbach's alpha coefficient (0.806).
Procedures
The data collection process began with obtaining the project acceptance documents.
Direct contact was made with each of the older adults so that after an explanation of the study they decided to take part in the study, as evidenced by the signing of an informed consent form.
Those who agreed to participate were given the instrument (questionnaire), which was previously coded to maintain anonymity.
All data were entered into a spreadsheet to proceed with the analysis.
Statistical analysis
The SPSS 25 program was used, and then quality control was carried out by means of consistency and purification of records. Absolute and relative frequencies were used to describe qualitative variables and quantitative variables. The determination of the factors associated with quality of life in older adults with advanced chronic organ failure was carried out using the Chi-square test and the calculation of the PR (Simple Prevalence Ratio) to identify the factors with the highest probability of risk. After that, by means of multivariate analysis corresponding to Poisson regression, all the significant factors that were finally associated with the variable of interest were influenced. In addition. The RPa (adjusted prevalence ratio) and 95% confidence intervals were determined. A significance level of 5% was taken into account, i.e. a p-value of less than 0.05 was significant..
Ethical aspects
Authorization for this study was requested and obtained from the Teaching and Research Support Office (Memorandum No. 012 and No. 124), as well as from the Research Division (Memorandum No. 259) and the Geriatrics Service (Memorandum No. 283) of the "Cirujano Mayor Santiago Távara" Naval Medical Center. Likewise, the ethical principles were complied with, based on the bioethical guidelines of the Declaration of Helsinki26, i.e., the confidentiality of the patients was respected, keeping their personal data anonymous, and there was no risk for the inappropriate use of the information, thus respecting the principle of non-maleficence.
RESULTS
It was observed that (44) 44% of older adults were over 80 years old, (59) 59% were male, (30) 30% studied up to secondary level, (57) 57% were incumbents in the navy, comorbidities were observed as arterial hypertension (74) 74%, diabetes mellitus (34) 34%, hypothyroidism (15) 15%, among others, and (83) 83% had advanced chronic organ failure for more than one year (Table 1).
Table 1. Epidemiological factors of older adults seen at the "Cirujano Mayor Santiago Távara" Naval Medical Center between April and July 2021.
| Epidemiological factors | N=100 | % |
| Age group | ||
| 60 to 69 years old | 23 | 23.0% |
| 70 to 79 years | 33 | 33.0% |
| >80 years | 44 | 44.0% |
| Sex | ||
| Male | 59 | 59.0% |
| Female | 41 | 41.0% |
| Level of education | ||
| Illiterate | 2 | 2.0% |
| Primary | 20 | 20.0% |
| Secondary | 30 | 30.0% |
| Superior technology | 31 | 31.0% |
| Superior | 17 | 17.0% |
| Relationship with the navy | ||
| Holder | 57 | 57.0% |
| Family | 43 | 43.0% |
| Comorbidities | ||
| Arterial hypertension | 74 | 74.0% |
| Diabetes mellitus | 34 | 34.0% |
| Hyperthyroidism | 15 | 15.0% |
| Arterial insufficiency | 2 | 2.0% |
| Others | 48 | 48.0% |
| Time of illness | ||
| <6 months | 5 | 5.0% |
| 6 months to 1 year | 12 | 12.0% |
| > 1 year | 83 | 83.0% |
Among the most frequent geriatric syndromes in older adults were visual or hearing deficits (82) 82%, insomnia (59) 59%, constipation (52) 52%, malnutrition (47) 47%, fall in the last year (27) 27% and pressure injury (13) 13%. On the other hand, mild functional dependence was observed in (48) 48% of the older adults, severe dependence in (50) 50% and total dependence in (2) 2% (Tabla 2)
Table 2. Geriatric syndromes and functional dependence in older adults seen at the "Cirujano Mayor Santiago Távara" Naval Medical Center from April to July 2021.
| Geriatric syndromes | N | % |
| Visual or hearing impairment | ||
| Yes | 82 | 82.0% |
| No | 18 | 18.0% |
| Insomnia | ||
| Yes | 59 | 59.0% |
| No | 41 | 41.0% |
| Constipation | ||
| Yes | 52 | 52.0% |
| No | 48 | 48.0% |
| Malnutrition | ||
| Yes | 47 | 47.0% |
| No | 53 | 53.0% |
| Fall | ||
| Yes | 27 | 27.0% |
| No | 73 | 73.0% |
| Pressure injury | ||
| Yes | 13 | 13.0% |
| No | 87 | 87.0% |
| Functional dependence | ||
| Total dependence | 2 | 2.0% |
| Severe dependence | 50 | 50.0% |
| Mild dependence | 48 | 48.0% |
| Total | 100 | 100.0% |
Figure 1 shows that 34% of older adults had a low quality of life, 63% had a medium quality of life and only 3% had a high quality of life.
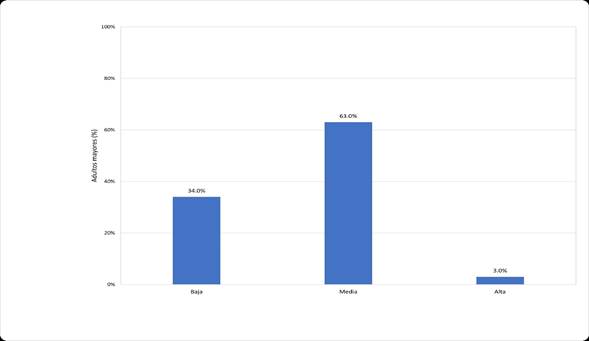
Figure 1: Quality of life of older adults attended at the "Cirujano Mayor Santiago Távara" Naval Medical Center from April to July 2021. Source: obtained from application of the WHOQoL-Bref questionnaire
Among the epidemiological factors related to low quality of life, it was found that age over 80 years (p = 0.032, PR = 1.818), female sex (p = 0.009, PR = 2.056), the degree of education given by illiteracy, primary and secondary (p = 0.025, PR = 1.930) and the relationship with the navy as family (p = 0.022, PR = 1.894) (Table 3).
Table 3. Epidemiological factors and quality of life of older adults attended at the "Cirujano Mayor Santiago Távara" Naval Medical Center from April to July 2021.
| Epidemiological factors | Low quality of life (n, %) | P* | Rp** | Ci (95%) *** |
| Age | ||||
| 60 to 69 years old | 5 (14.7%) | 0.157 | Ref. | |
| 70 to 79 years | 9 (26.5%) | 0.319 | 0.731 | 0.38 - 1.38 |
| > 80 years | 20 (58.8%) | 0.032 | 1.818 | 1.04 - 3.17 |
| Sex | ||||
| Female | 20 (58.8%) | 0.009 | 2.056 | 1.18 - 3.58 |
| Male | 14 (41.2%) | |||
| Level of education | ||||
| Illiterate/primary/high school | 23 (67.6%) | 0.025 | 1.930 | 1.05 - 3.52 |
| Superior/superior technique | 11 (32.4%) | |||
| Relationship with the navy | ||||
| Family | 20 (58.8%) | 0.022 | 1.894 | 1.08 -3.30 |
| Holder | 14 (41.2%) | |||
| Diagnosis | ||||
| Advanced heart failure | 6 (17.6%) | 0.804 | 0.914 | 0.44 - 1.88 |
| Advanced chronic kidney disease | 15 (44.1%) | 0.483 | 0.822 | 0.47 - 1.42 |
| Advanced respiratory failure | 9 (26.5%) | 0.114 | 1.640 | 0.93 - 2.88 |
| Advanced cirrhosis | 4 (11.8%) | 0.644 | 0.819 | 0.34 - 1.96 |
| Comorbidities | ||||
| Arterial hypertension | 27 (79.4%) | 0.376 | 1.355 | 0.67 - 2.73 |
| Diabetes mellitus | 12 (35.3%) | 0.845 | 1.059 | 0.59 - 1.87 |
| Arterial insufficiency | 1 (2.9%) | 0.629 | 1.485 | 0.36 - 6.10 |
| Hyperthyroidism | 6 (17.6%) | 0.595 | 1.214 | 0.60 - 2.42 |
| Others | 20 (58.8%) | 0.120 | 1.548 | 0.88 - 2.70 |
| Time of illness | ||||
| <6 months | 1 (2.9%) | 0.498 | Ref. | |
| 6 months to 1 year | 3 (8.8%) | 0.483 | 0.710 | 0.25 - 1.96 |
| >1 year | 30 (88.2%) | 0.317 | 1.536 | 0.62 - 3.79 |
*p: chi-square test, **RP: prevalence ratio, ***IC (95%): confidence interval.
Insomnia (p=0.034, PR=1.930), constipation (p=0.000, PR=3.560), pressure injury (p=0.000, PR=2.788) and severe functional dependence (p=0.000, PR=4.667) were geriatric syndromes associated with low quality of life (Table 4).
Table 4. Geriatric syndromes and quality of life of older adults seen at the "Cirujano Mayor Santiago Távara" Naval Medical Center from April to July 2021.
| Geriatric syndromes | Low quality of life (n, %) | P | Rp | Ci (95%) |
| Visual or hearing impairment | ||||
| Yes | 29 (85.3%) | 0.538 | 1.273 | 0.57 - 2.83 |
| No | 5 (14.7%) | |||
| Insomnia | ||||
| Yes | 25 (73.5%) | 0.034 | 1.930 | 1.00 - 3.69 |
| No | 9 (26.5%) | |||
| Constipation | ||||
| Yes | 27 (79.4%) | 0.000 | 3.560 | 1.71 - 7.41 |
| No | 7 (20.6%) | |||
| Malnutrition | ||||
| Yes | 19 (55.9%) | 0.201 | 1.428 | 0.82 - 2.48 |
| No | 15 (44.1%) | |||
| Fall | ||||
| Yes | 12 (35.3%) | 0.180 | 1.475 | 0.85 - 2.55 |
| No | 22 (64.7%) | |||
| Pressure injury | ||||
| Yes | 10 (29.4%) | 0.000 | 2.788 | 1.77 - 4.38 |
| No | 24 (70.6%) | |||
| Functional dependence | ||||
| Total dependence | 1 (2.9%) | 0.629 | 1.485 | 0.36 - 6.10 |
| Severe dependence | 28 (82.4%) | 0.000 | 4.667 | 2.12 - 10.28 |
| Mild dependence | 5 (14.7%) | 0.000 | Ref. |
*p: chi-square test, **pr: prevalence ratio, ***ic (95%): 95% confidence interval.
Finally, multivariate analysis showed that insomnia (p=0.002), pressure injury (p=0.016) and severe dependence (p=0.000) were the factors associated with quality of life in older adults attended at the "Cirujano Mayor Santiago Távara" Naval Medical Center (Table 5).
Table 5. Multivariate analysis of the factors associated with the quality of life of older adults attended at the "Cirujano Mayor Santiago Távara" Naval Medical Center between April to July 2021
| Associated factors | B | P | Rpa | Ci (95%) | |
| Inferior | Superior | ||||
| (intersection) | 0.643 | 0.001 | 0.526 | 0.35 | 0.78 |
| Age > 80 years | 0.039 | 0.436 | 1.039 | 0.94 | 1.15 |
| Sex | 0.032 | 0.612 | 1.032 | 0.91 | 1.17 |
| Level of education: Illiterate/primary/high school | 0.038 | 0.429 | 1.039 | 0.95 | 1.14 |
| Relationship with marina de war: family | 0.007 | 0.899 | 1.007 | 0.90 | 1.12 |
| Insomnia | 0.153 | 0.002 | 1.166 | 1.06 | 1.28 |
| Constipation | 0.023 | 0.652 | 1.023 | 0.92 | 1.13 |
| Pressure injury | 0.221 | 0.016 | 1.248 | 1.04 | 1.49 |
| Severe dependency | 0.188 | 0.000 | 1.207 | 1.09 | 1.33 |
Dependent variable: quality of life *b: coefficient, p: significance value, rpa: adjusted prevalence ratio, ci (95%): 95% confidence interval.
Model: (intersection), age > 80 years, sex, education level, relationship to navy, insomnia, constipation, pressure injury, severe dependence.
DISCUSSION
When analyzing 100 patients, it was possible to identify that most of the older adults had a medium quality of life, followed by those with a low quality of life, which coincides with the majority of related studies, both in the national and international environment27,28,20. This would show that older adults, regardless of the geographical area in which they are, will have a quality of life related to the state in which they are, because sometimes they may have deficiencies generated by the physiological deterioration that occurs at this stage of life.
Bivariate and non-multivariate epidemiological factors associated with low quality of life in older adults were found to be age >80 years, as found by Vega29who, when analyzing older adults with diabetes mellitus in Cajamarca, found that age between 70 and 79 years (p=0.001) was related to this level of quality of life, a similar situation was identified by Valdés30who, after analyzing older adults in a health center in Arequipa, found that people aged 76-84 years (p=0.026) had a low quality of life. Thus, it could be said that the older the person is, the greater the deterioration of his or her quality of life will be. This could be due to the deterioration of their physiological and functional state, causing disability and limitations to perform their activities autonomously, leading to a decline in their quality of life31.
Another factor identified as associated with low quality of life, in a bivariate manner, was the degree of illiteracy/primary/secondary education. Similar results were found in related studies, which demonstrate that low educational level (p=0.000)29as well as illiteracy (p=0.033)30. This could be explained by the fact that the absence or lack of information on the importance of controlling comorbidities is a major limitation for self-care, since preventive measures are not applied, which is reflected in the low quality of life32,33.
Being a family member of a Navy officer was the last bivariate epidemiological factor for a low quality of life. No studies have been found on this variable that affirm or contradict it, since studies in military institutions have not been identified. Other studies have been able to identify variables that have been considered as factors for low quality of life, these being male sex34and widowed marital status29.
In addition, insomnia and the presence of pressure sores were the geriatric syndromes that were independently associated with low quality of life. No studies have been found, both nationally and internationally, that have correlated these variables with quality of life, finding not only a lack of information, but also an opportunity for further research in this regard.
In relation to functional dependence, severe functional dependence was found to be an independent factor for low quality of life. Several studies also found this correlation in the international setting, such as Laredo et al.28, which found in Mexican older adults that those with functional dependence were those who mainly had low quality of life, or in the national setting, where Castillo et al.35, after carrying out his study in Juliaca, concluded that functional dependence had a significant influence on quality of life (p=0.000); a situation similar to that reported by Salluca and Velasquez36who demonstrated the association of both variables in a significant and directly proportional manner. These associations are usually significant because when older adult has difficulty in performing their daily activities, is no longer fully autonomous, and cannot perform their roles, social and family tasks; they influence the impairment of their quality of life.28
Subsequently, studies have analyzed the possible relationship between other variables and quality of life, such as the study by Polku et al.37who found that perceived hearing difficulty was significantly associated with the overall quality of life score evaluated with the WHO short version, as well as with each of its domains (physical, psychological, social and environmental). While Liu et al.38evaluating Chinese elderly, found that the greater the number of non-communicable diseases (NCDs) in the elderly, the greater the deterioration of quality of life, measured with the Chinese version of the Quality of Life-Old (1 NCD p<0.05, 2 NCDs and 3 to more NCDs p<0.001, respectively). And Kantow et al.39, when analyzing older adults in northern Thailand identified that awareness of falls and falls itself were associated with quality of life, where those older adults who had a history of falling in the previous year had lower quality of life (p<0.001). With these studies it can be mentioned that various factors influence quality of life in older adults, that is, it is multifactorial, so it is relevant to expand the evidence both nationally and locally, with a broader population to identify those other factors that are involved in the reduction of this quality of life.
And Kantow et al.39, when analyzing older adults in northern Thailand identified that awareness of falls and falls itself were associated with quality of life, where those older adults who had a history of falling in the previous year had lower quality of life (p<0.001). With these studies it can be mentioned that various factors influence quality of life in older adults, that is, it is multifactorial, so it is relevant to expand the evidence both nationally and locally, with a broader population to identify those other factors that are involved in the reduction of this quality of life.
The limitations found for this study is that there is scarce evidence and studies on organ failure and in the advanced stage under the same methodological approach, which influenced the adequate comparison of data with other environments. The evaluation of the quality of life in older people with advanced chronic organ failure is limited in general. The surveys limit their population to individuals suffering from specific pathologies, limiting the contrast, as is done in the present study.
Finally, it is concluded that insomnia, pressure injury, and severe functional dependence are factors associated with low quality of life in older adults with advanced chronic organ failure in a hospital in Lima-Peru.
REFERENCES
1. De pina r, aparecido m, de sousa a, pilotto m, kusumota l. Quality of life of elderly people with chronic kidney disease in conservative treatment. Rev bras enferm. 2017; 70(4): 851-859. Doi: 10.1590/0034-7167-2017-0103 [ Links ]
2. Fuentes l, padrón d, libreros l. Indicadores de envejecimiento demográfico del estado de carabobo, venezuela. Periodo 1990-2011. Comunidad y salud. 2017; 15(1): 20-29. Disponible en: http://ve.scielo.org/scielo.php?script=sci_arttext&pid=s1690-32932017000100004 [ Links ]
3. Martínez t, gonzález c, castellón g, gonzález b. El envejecimiento, la vejez y la calidad de vida: ¿éxito o dificultad? Rev finlay. 2018; 8(1): 59-65. Disponible en: http://scielo.sld.cu/scielo.php?pid=s2221-24342018000100007&script=sci_abstract&tlng=es [ Links ]
4. Rivillas j, gómez-artistizabal l, rengifo-reina h, muñoz-laverde e. Envejecimiento poblacional y desigualdades sociales en la mortalidad del adulto mayor en colombia. Rev fac nac salud pública. 2017; 35(2): 369-381. Doi: 10.17533/udea.rfnsp.v35n3a07 [ Links ]
5. Organización mundial de la salud. Envejecimiento y salud. Who. [online].; 2021. [revisado el 28 de octubre del 2021]. Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/envejecimiento-y-salud [ Links ]
6. Ministerio de sanidad, servicios sociales e igualdad. Las personas mayores opinan sobre la salud y el bienestar en países de ingresos medios y bajos que envejecen a un ritmo acelerado. Envejecimiento y salud. Barcelona: gobierno de españa, secreataría de estado de servicios sociales e igualdad; 2019. [ Links ]
7. Blay c, martori j, limón e, oller r, vila l, gómez-batiste x. Busca tu 1%: prevalencia y mortalidad de una cohorte comunitaria de personas con enfermedad crónica avanzada y necesidades paliativas. Aten primaria. 2019; 51(2): 71-79. Doi: 10.1016/j.aprim.2017.07.004 [ Links ]
8. Blay c, martori j, limon e, lasmarías c, oller r, gómez x. Cada semana cuenta: uso de dispositivos sanitarios y costes relacionados de un cohorte comunitaria de personas con enfermedades crónicas avanzadas. Aten primaria. 2018; 1(1): 1-8. Doi: 10.1016%2fj.aprim.2018.03.008 [ Links ]
9. Jesus n, ferreira g, mendes-rodrigues c, de almeida o, dias d, martins c. Quality of life of individuals with chronic kidney disease on dialysis. Braz j nephrol. 2019; 41(3): 364-374. Doi: 10.1590/2175-8239-jbn-2018-0152 [ Links ]
10. Labenz c, toenges g, schattenberg j, nagel m, huber y, marquardt j, et al. Health-related quality of life in patients with compensated and decompensated liver cirrhosis. Eur j intern med. 2019;(70): 54-59. Doi: 10.1016/j.ejim.2019.09.004 [ Links ]
11. Varela l. Salud y calidad de vida en el adulto mayor. Rev peru med exp salud publica. 2016; 33(2): 199-201. Doi: 10.17843/rpmesp.2016.332.2196 [ Links ]
12. Comín-colet j, anguita m, formiga f, almenar l, crespo-leiro m, manzano l, et al. Health-related quality of life of patients with chronic systolic. Heart failure in spain: results of the vida-ic study. Rev esp cardiol. 2016; 69(3): 256-271. Doi: 10.1016/j.rec.2015.07.030 [ Links ]
13. Zhou x, xue f, wang h, qiao y, liu g, huang l, et al. The quality of life and associated factors in patients on maintenance hemodialysis - a multicenter study in shanxi province. Ren fail. 2017; 39(1): 707-711. Doi: 10.1080/0886022x.2017.1398095 [ Links ]
14. Ñaupas h, valdivia m, palacios j, romero h. Metodología de la investigación cuantitativa - cualitativa y redacción de la tesis. 5th ed. México df: ediciones de la u; 2018. Disponible en: http://www.biblioteca.cij.gob.mx/archivos/materiales_de_consulta/drogas_de_abuso/articulos/metodologiainvestigacionnaupas.pdf [ Links ]
15. Hernández r, mendoza c. Metodología de la investigación ciudad de méxico: mc graw hill education; 2018. [ Links ]
16. Saldarriaga c, gómez e, navarrete s, gonzáles g, gómez j. Consenso colombiano para el diagnóstico y tratamiento de la insuficiencia cardiaca. [ Links ]
17. Blanco a, blázques j, boyano i. Epoc. Cor pulmonale. Tratado de geriatría para residentes. 2019; 1(1): 371-379. [ Links ]
18. Hospital cayetano heredia. Guía de práctica clínica para diagnóstico y tratamiento de insuficiencia renal crónica. Resolución directoral nº469-2017-hch/dg. 2017;: 1-15. Disponible en: http://www.hospitalcayetano.gob.pe/portalweb/wp-content/uploads/resoluciones/2017/rd/rd469-102017.pdf [ Links ]
19. Goldberg, e; runyon, b; robson, k. Cirrhosis in adults: etiologies, clinical manifestations, and diagnosis. [online].; 2018. [citado 2 setiembre 2020]. Disponible en: https://www.uptodate.com/contents/cirrhosis-in-adults-etiologies-clinical-manifestations-and-diagnosis?search=cirrosis&source=search_result&selectedtitle=1~150&usage_type=default&display_rank=1 [ Links ]
20. Alor r, milla e. Grado de dependencia y la callidad de vida de los pacientes adultos mayores del hospital naval-callao, 2019. [tesis de grado]. Lima : universidad peruana cayetano heredia; 2020. Disponible en: https://hdl.handle.net/20.500.12866/8130 [ Links ]
21. Delgado j. Caracterización clínico sociodemográfico y evaluación de estado funcional de pacientes geriátricos en el programa de atención domiciliaria del hospital ii essalud ilo, febrero del año 2019. [tesis de grado]. Tacna: universidad privada de tacna ; 2019. Disponible en: https://revistas.upt.edu.pe/ojs/index.php/etvita/article/view/158 [ Links ]
22. Hidalgo c, morales g, ortiz m, rojas m, bolboa t, lanuza f, et al. Propiedades psicométricas de la versión chilena del whoqol-bref para la calidad de vida. Psicología conductual. 2021; 29(2): 383-398. Disponible en: https://www.behavioralpsycho.com/wp-content/uploads/2021/09/10.hidalgo_29-2es.pdf [ Links ]
23. Espinoza i, osorio p, torrejón m, lucas r, bunout d. Validación del cuestionario de calidad de vida (whoqol-bref) en adultos mayores chilenos. Rev med chile. 2011;(139): 579-586. Doi: 10.4067/s0034-98872011000500003 [ Links ]
24. Mendoza n, roncal k. Calidad de vida del adulto mayor en el centro de salud callao, callao - 2016. Tesis de grado. Lima: universidad de ciencias y humanidades; 2018. Disponible en: https://repositorio.uch.edu.pe/handle/20.500.12872/195 [ Links ]
25. Cardona j, ospinza l, eljadue a. Validez discriminante, convergente/divergente, fiabilidad y consistencia interna, del whoqol-bref y el mossf-36 en adultos sanos de un municipio colombiano. Rev. Fac. Nac. Salud pública. 2015; 33(1): 50-57. Disponible en: http://www.scielo.org.co/scielo.php?script=sci_abstract&pid=s0120-386x2015000100007&lng=en&nrm=iso&tlng=es [ Links ]
26. Mazanti m. Declaración de helsinki, principios y valores bioéticos en juego en la investigación médica con seres humanos. Revista colombiana de bioética. 2011; 6(1): 125-144. Disponible en: https://www.redalyc.org/pdf/1892/189219032009.pdf [ Links ]
27. Levi j, castillo f, villa e. Perfil de calidad de vida del adulto mayor de los centros de adulto mayor en los distrito de chaclacayo y chosica, lima, Perú, 2014. Revista de investigación universitaria. 2015; 4(2): 57-63. Doi: 10.17162/riu.v4i2.686 [ Links ]
28. Loredo m, gallegos r, xeque a, palomé g, juárez a. Nivel de dependencia, autocuidado y calidad de vida del adulto mayor. Enfermería universitaria. 2016; 13(3): 159-165. Disponible en: https://www.scielo.org.mx/pdf/eu/v13n3/1665-7063-eu-13-03-00159.pdf [ Links ]
29. Vega m. Calidad de vida y los factores biosociales del adulto mayor con diabetes mellitus tipo ii. Essalud. Cajamarca, 2015. [tesis de grado]. Universidad nacional de cajamarca ; 2017. Disponible en: https://repositorio.unc.edu.pe/handle/20.500.14074/914 [ Links ]
30. Valdez j. Factores psicológicos y sociales relacionados a la calidad de vida del adulto mayor, centro de salud cono sur i-4, san roman 2017. [tesis de grado]. Universidad nacional del altiplano; 2018. Disponible en: https://tesis.unap.edu.pe/bitstream/handle/20.500.14082/6975/valdez_condori_jackeline_vanesa.pdf?sequence=1&isallowed=y [ Links ]
31. Long m, pons s, delgado v, oliva m, tamayo y, gonzález j. Apreciación de la calidad de vida en el adulto mayor. Multimed. Revista médica. Granma. 2018; 1(1): 1-12. Disponible en: https://revmultimed.sld.cu/index.php/mtm/article/view/777 [ Links ]
32. Herrera j. Calidad de vida del adulto mayor con hipertensión arerial essalud - distrito de chota, 2017. [tesis de grado]. Universidad nacional de cajamarca; 2019. Disponible en: https://repositorio.unc.edu.pe/handle/20.500.14074/3504 [ Links ]
33. Herrera j, oblitas a. Calidad de vida del adulto mayor hipertenso. Chota, 2017. Acc cietna. 2020; 7(1): 31-41. Doi: 10.35383/cietna.v7i1.354 [ Links ]
34. Martínez o, camarero o, gonzález c, martínez l. Calidad de vida del adultos mayor en un consultorio médico del municipio jaruco. Revista de ciencias médicas. La habana. 2016; 22(1): 30-41. Disponible en: https://www.medigraphic.com/cgi-bin/new/resumen.cgi?idarticulo=66018 [ Links ]
35. Castillo m. Dependencia funcional y su influencia en la calidad de vida, en usuarios de la casa del adulto mayor, cerro colorado arequipa, noviembre 2017- enero 2018. [tesis de grado]. Universidad andina "néstor cáceres velásquez"; 2018. Disponible en: http://repositorio.uancv.edu.pe/bitstream/handle/uancv/2970/t036_72144027_t.pdf?sequence=3&isallowed=y [ Links ]
36. Salluca m, velásquez m. Calidad de vida y capacidad funcional del adulto mayor hospitalizado en la unidad de ortogeriatría de un hospital del callao-2018. [tesis de grado]. Universidad norbert wiener; 2019. Disponible en: https://repositorio.uwiener.edu.pe/bitstream/handle/20.500.13053/2662/tesis%20salluca%20maria%20-%20vel%c3%a1squez%20mar%c3%ada.pdf?sequence=1 [ Links ]
37. Polku h, mikkola t, rantakokko m, portegijs e, tormakangas t, rantanen t, et al. Hearing and quality of life among community-dwelling older adults. J gerontol b psychol sci soc sc. 2018; 73(3): 543-552. Doi: 10.1093/geronb/gbw045 [ Links ]
38. Liu j, yu w, zhou j, chen s, wu s. Relationship between the number of noncommunicable diseases and health-related quality of life in chinese older adults: a cross-sectional survey. Int j environ res public health. 2020; 17(14): 5150. Doi: 10.3390/ijerph17145150 [ Links ]
39. Kantow s, seangpraw k, ong-artborirak p, tonchoy p, auttama n, bootsikeaw s, et al. Risk factors associated with fall awareness, falls, and quality of life among ethnic minority older adults in upper northern thailand. Clin interv aging. 2021; 16(1): 1777-1788. Doi: 10.2147/cia.s328912 [ Links ]
8 Article published by the journal of the faculty of human medicine of the ricardo palma university. It is an open access article, distributed under the terms of the creatvie commons license: creative commons attribution 4.0 international, cc by 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: March 21, 2023; Accepted: May 22, 2023











 texto en
texto en 


