Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.23 no.3 Lima jul./set. 2023 Epub 21-Sep-2023
http://dx.doi.org/10.25176/rfmh.v23i3.5846
Original Article
First report of a dengue outbreak in balsas, Amazonas, Peru, during 2021 and 2022
1Instituto de Enfermedades Tropicales, Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas (UNTRM), Amazonas, Peru.
2Laboratorio Referencial de Salud Pública Amazonas, Dirección Regional de Salud Amazonas, Peru.
3Faculty of Human Medicine, Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas, Amazonas, Peru.
4Instituto de Investigaciones en Ciencias Biomédicas (INICIB), Universidad Ricardo Palma, Lima, Peru.
Introduction:
The increase in dengue cases in Amazonas represents a public health risk. In 2021, Balsas reported a dengue outbreak for the first time.
Methods:
The population included patients who met the case definition between December 2021 and February 2022. Serotype identification was determined using a multiplex qRT-PCR.
Results:
A total of 72 patients were identified, of which 53 (74%) were confirmed by serology (NS1 Ag). The prevalent serotype was DENV-2 (94%), and 6% were DENV-1. Patients aged 19 to 45 years had the highest percentage of cases (59%). The most frequent symptoms were headache, myalgia, fever, and arthralgia; 23% had intense abdominal pain.
Conclusion:
This was the first confirmed dengue outbreak in the Balsas district, with DENV-2 being the main cause of the outbreak, highlighting the need to improve surveillance in areas without autochthonous transmission of the disease.
Keywords: Dengue; Serotype; Outbreak
INTRODUCTION
Dengue is one of the most significant arboviruses globally, primarily transmitted by the Aedes aegypti vector, which spreads in tropical and subtropical regions, causing socioeconomic and health impacts1,2. The dengue virus belongs to the flaviviridae family and is divided into 4 serotypes (DENV-1, DENV-2, DENV-3, DENV-4), which are further subdivided into phylogenetically distinct genotypes3.
Dengue has been circulating in Peru since 1990 and presented an epidemic caused by the DENV-1 serotype in the city of Iquitos, marking the first laboratory-confirmed case of autochthonous transmission in the country. Another smaller outbreak occurred in Tarapoto, and data indicates that the same dengue serotype was involved in both outbreaks4. Subsequently, larger and smaller outbreaks occurred in various areas of the country. Dengue incidence in recent years has been primarily restricted to the northern part of the country and much of the Amazon5. In 2019, the introduction of the Cosmopolitan genotype of the DENV-2 serotype was first detected in the Madre de Dios region of Peru2. Genomic surveillance of this genotype is vital as its genomic diversity, evolution, and transmission dynamics are still unknown3. Recently, Peru has experienced an increase in the number of dengue cases, with 44,791 cases reported in 2021 and 63,168 in 2022, with Amazonas being one of the most affected regions. In 2020, there were 845 reported cases, increasing to 2,304 in 2021, and further to 3,502 in 20225.
The unusual increase in dengue cases in the Amazonas region poses a significant risk to public health due to the lack of a proper vector prevention and control system. In December 2021, the district of Balsas in the Chachapoyas province reported its first cases of dengue following a magnitude 7.5 earthquake in the department6. This earthquake may have been a factor contributing to the emergence of reemerging diseases like dengue due to the absence of an adequate epidemiological surveillance system. To date, Balsas is the first and only district in this province to report autochthonous dengue cases. The ability of the Aedes aegypti vector to infest new locations and adapt to climate changes, even after natural disasters, has been substantial in the transmission, establishment, and spread of the disease. The objective of this study was to describe the first dengue outbreak in Balsas, its clinical-epidemiological characteristics, and the circulating serotypes.
METHODS
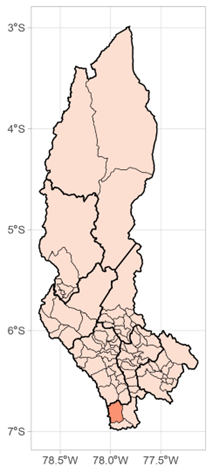
The district of Balsas has a population of 1,158 inhabitants and is located in the southwest of the Chachapoyas province (Figure 1). It includes 20 populated centers. The presence of the vector was only evidenced in the populated center of Balsas, which has 6 annexes and comprises 676 inhabitants (58% of the total population). It is situated at an altitude of 859 meters above sea level, has a warm-humid climate, and temperatures ranging from 11°C to 35°C with an annual average of 20°C. The rainy season occurs between October and May, with an annual precipitation of 780 mm7, providing ideal climatic conditions for vector development.
Figure 1. Geo-Referential Map of Balsas District in the Chachapoyas Province, Amazonas Department.
A descriptive study was conducted. The Amazonas Regional Health Directorate (DIRESA) conducted active and passive surveillance, with some cases confirmed only through epidemiological linkage. The study population included all patients meeting the dengue case definition8between December 2021 and February 2022 in the populated center of Balsas, excluding patients without samples for serological diagnosis. Demographic, clinical, epidemiological, and laboratory data were obtained from clinical-epidemiological research forms collected by DIRESA-Amazonas. RNA extraction from serum samples of patients who tested positive for the NS1 antigen serological diagnosis was performed manually using the silica column method, following the instructions of the Viral Nucleic Acid extraction II kit (Geneaid®). The identified serotypes were determined using a qRT-PCR multiplex based on the protocol established by the Instituto Nacional de Salud, using the TransScript II Multiplex Probe One-Step qRT-PCR SuperMix UDG kit. The amplification process was carried out in the Quant Studio 5 thermocycler. Data were imported into an Excel database, and data reliability was verified through duplication. Frequencies, percentages, and ranges were used for statistical analysis with STATA v17 software. This study is part of the METAVEC project with contract No. 050-2021-FONDECYT, which has approval from the Institutional Research Ethics Committee of the Universidad Nacional Toribio Rodríguez de Mendoza de Amazonas, with certificate No. 011. This study is part of the surveillance activities carried out by DIRESA - Amazonas, and the necessary permissions were obtained.
RESULTS
Dengue was introduced into the district of Balsas in December 2021, with the first confirmed case reported on December 28th in a laboratory healthcare worker. In this outbreak, 72 patients who met the dengue case definition were identified, of which 53 (74%) were confirmed by serology (NS1 Ag). The percentage of females was slightly higher (53%), and the median age was 37 years [IQR 23 - 53.5 years], with the age range of 19 to 45 years having the highest percentage of cases (59%) (Table 1). Regarding clinical-epidemiological characteristics, the most frequent symptoms were headache and myalgia (90.6%), fever (89%), and arthralgia (75.5%); 23% presented intense abdominal pain (warning sign). 58.5% of cases were diagnosed within 2 days or less of symptoms, while 15% were diagnosed between 6 and 8 days of symptoms, with a median of 1 day [IQR 1 - 2 days]. 38% of cases had 5 or fewer days between the onset of symptoms and the confirmation of the dengue case, while 49% had between 6 and 9 days, with a median of 2 days [IQR 1 - 2 days] (Table 2). The circulating serotypes in this outbreak were DENV-2 (94%) and DENV-1 (6%).
Table 1. Sociodemographic characteristics of the population
| Variable | Positive (%) | Negative (%) | Total |
| Gender | |||
| Male | 25 (65.8) | 13 (34.2) | 38 |
| Female | 28 (82.4) | 6 (17.6) | 34 |
| Age | |||
| ≤ 18 | 7 (63.6) | 4 (36.4) | 11 |
| 19 - 45 | 31 (83.8) | 6 (16.2) | 37 |
| ≥ 46 | 15 (62.5) | 9 (37.5) | 24 |
| Education level | |||
| Primary | 4 (50.0) | 4 (50.0) | 8 |
| Secondary | 28 (68.3) | 13 (31.7) | 41 |
| Higher | 21 (91.3) | 2 (8.7) | 23 |
| Occupation | |||
| At home | 28 (80.0) | 7 (20.0) | 35 |
| Outside home | 25 (67.6) | 12 (32.4) | 37 |
Table 2. Clinical Characteristics of the Population
| Variable | Positive (%) | Negative (%) | Total |
| Days of symptoms | |||
| ≤ 2 | 31 (73.8) | 11 (26.2) | 42 |
| 3 - 5 | 14 (66.7) | 7 (33.3) | 21 |
| ≥ 6 | 8 (88.9) | 1 (11.1) | 9 |
| Days of result | |||
| ≤ 5 | 20 (62.5) | 12 (37.5) | 32 |
| 6 - 9 | 26 (78.8) | 7 (21.2) | 33 |
| ≥ 10 | 7 (100) | 0 | 7 |
| Fever | |||
| Yes | 47 (75.8) | 15 (24.2) | 62 |
| No | 6 (60.0) | 4 (40.0) | 10 |
| Arthralgia | |||
| Yes | 40 (83.3) | 8 (16.7) | 48 |
| No | 13 (54.2) | 11 (45.8) | 24 |
| Myalgia | |||
| Yes | 48 (77.4) | 14 (22.6) | 62 |
| No | 5 (50.0) | 5 (50.0) | 10 |
| Headache | |||
| Yes | 48 (72.7) | 18 (27.3) | 66 |
| No | 5 (83.3) | 1 (16.7) | 6 |
| Ocular pain | |||
| Yes | 38 (79.2) | 10 (20.8) | 48 |
| No | 15 (62.5) | 9 (37.5) | 24 |
| Lumbar pain | |||
| Yes | 35 (79.6) | 9 (20.4) | 44 |
| No | 18 (64.3) | 10 (35.7) | 28 |
| Rash | |||
| Yes | 11 (91.7) | 1 (8.3) | 12 |
| No | 42 (70.0) | 18 (30.0) | 60 |
| Non-Purulent Conjunctivitis | |||
| Yes | 12 (92.3) | 1 (7.7) | 13 |
| No | 41 (69.5) | 18 (30.5) | 59 |
| Nausea/Vomiting | |||
| Yes | 29 (76.3) | 9 (23.7) | 38 |
| No | 24 (70.6) | 10 (29.4) | 34 |
| Case classification | |||
| Without warning signs | 39 (68.4) | 18 (31.6) | 57 |
| With warning signs | 14 (93.3) | 1 (6.7) | 15 |
DISCUSSION
Environmental-climatic phenomena are related to dengue outbreaks and play a role in the survival, behavior, and reproduction of the Aedes aegypti vector1. In November 2021, an earthquake occurred, causing environmental-climatic disruptions in the Amazonas region6, leading to flooding due to heavy rains and the overflow of the Utcubamba River, creating an environment conducive to the emergence of diseases. This natural disaster disrupted the main road, causing increased human mobility, with Balsas serving as the access route for transportation and trade. Increased population movement and vector dissemination are factors contributing to disease establishment9. In this outbreak, 53 cases of dengue were confirmed, representing 7% of the population in the populated center of Balsas. Other suspected dengue cases could not be confirmed due to residents' refusal to provide samples and a shortage of healthcare workers to handle cases. Dengue infections can affect a significant portion of the population in a short period during an epidemic, leading to adverse economic consequences and potential healthcare system overload. The dengue virus affects all age groups in different proportions and with different clinical presentations. While younger than 15 years and older than 60 years are the most vulnerable age groups, studies have reported a higher frequency of dengue cases in the 16 to 45-year age group9,10. In this outbreak, the most affected age group ranged from 19 to 45 years, possibly because adults engage in more daytime activities and are thus more exposed to vector bites, resulting in a higher infection rate. Clinical manifestations of dengue vary, ranging from asymptomatic infections to mild and severe classic cases, and in some instances, hemorrhagic cases, which can be fatal11. While there are limited studies evaluating differences in clinical presentations based on serotypes, currently, DENV-2 is more strongly associated with cases exhibiting greater symptoms and severity worldwide12. In our study, no hospitalizations or severe cases were reported, likely because all cases were first-time dengue infections. The most common symptoms found were headache, myalgia, fever, and arthralgia10,13. It was also noted that only 23% of cases presented intense abdominal pain related to one of the four warning signs(14. The majority of cases were diagnosed within two or fewer days of symptoms (58.5%), contributing to early symptom treatment and a better prognosis for the disease15. The confirmed circulating serotypes in this study were DENV-1 and DENV-2, with the latter being the primary cause of most infections. This serotype predominates in various regions of Asia and has gradually spread to other parts of the world16. The co-circulation of two or more serotypes is important because it results in specific immunity for each serotype, making individuals susceptible to a second infection by a different serotype, thus maintaining virus transmission17. Recent reports have indicated the presence of a new DENV-2 serotype genotype in the Americas, the Cosmopolitan genotype, which was first reported in Madre de Dios, Peru, and two years later in Brazil. This serotype circulates globally and exhibits a wide range of genotypic dispersion patterns, which may explain the rapid increase in the incidence and prevalence of the DENV-2 serotype2,3,16. This study was limited by the small sample size, which prevented statistical analysis of associations with serotypes and clinical variables, as well as the low severity of cases due to them being primary infections. Therefore, there is a need to improve surveillance systems in healthcare facilities in areas without autochthonous transmission of the disease, and integrated vector control strategies and timely case detection should be implemented. Due to the outbreaks of DENV-2, genomic surveillance is important to assess the impact on the transmission and spread of predominant serotypes and genotypes. This is crucial for disease control at the local and regional levels.
REFERENCES
1. Dostal T, Meisner J, Munayco C, García PJ, Cárcamo C, Pérez JE, et al. The effect of weather and climate on dengue outbreak risk in Peru, 2000-2018: A time-series analysis. PLoS Negl Trop Dis [internet]. 2022 [citado el 03 de julio de 2023]; 16(6), e0010479. doi: https://doi.org/10.1371/journal.pntd.0010479 [ Links ]
2. García MP, Padilla C, Figueroa D, Manrique C, Cabezas C. Emergencia del genotipo Cosmopolitan del virus dengue serotipo 2 (DENV2) en Madre de Dios, Perú, 2019. Rev Peru Med Exp Salud Pública. 2022; 39(1):126-128. doi: https://doi.org/10.17843/rpmesp.2022.391.10861 [ Links ]
3. Giovanetti M, Pereira LA, Santiago GA, Fonseca V, García-Mendoza M, de Oliveira C, et al. Emergence of Dengue Virus Serotype 2 Cosmopolitan Genotype, Brazil. Emerg Infect Dis. 2022; 28(8):1725-1727. doi: https://doi.org/10.3201/eid2808.220550 [ Links ]
4. Cabezas C, Fiestas V, García MP, Palomino M, Mamani E, Donaires F. Dengue en el Perú: a un cuarto de siglo de su reemergencia. Rev Peru Med Exp Salud Pública. 2015; 32(1):146-156. Disponible en: https://www.scielosp.org/article/ssm/content/raw/?resource_ssm_path=/media/assets/rpmesp/v32n1/a21v32n1.pdf [ Links ]
5. Centro Nacional de Epidemiologia, Prevención y Control de Enfermedades - MINSA. Sala Situacional de Dengue [Internet]. Sala situacional [consultado el 3 de julio del 2023]. Disponible en: https://www.dge.gob.pe/sala-situacional-dengue/#grafico02 [ Links ]
6. Instituto Geofísico del Perú - MINAM. Reporte Sísmico: IGP/CENSIS/RS 2021-0754 [Internet]. Centro Sismológico Nacional [consultado el 31 de julio del 2023]. Disponible en: https://ultimosismo.igp.gob.pe/evento/2021-0754 [ Links ]
7. Gobierno del Perú. Distrito de Balsas [Internet]. Ciudades y Distritos del Perú [consultado el 4 de julio del 2023]. Disponible en: https://www.distrito.pe/distrito-balsas.html [ Links ]
8. Ministerio de Salud del Perú. Norma técnica De Salud Para La Vigilancia Epidemiológica Y Diagnóstico De Laboratorio de Dengue, Chikungunya, Zika y otras Arbovirosis en el Perú [Internet]. Plataforma digital única del Estado Peruano [consultado el 31 de julio del 2023]. Disponible en: https://www.gob.pe/institucion/minsa/normas-legales/191438-982-2016 [ Links ]
9. Ali A, Ahmad H, Idrees M, Zahir F, Ali I. Circulating serotypes of dengue virus and their incursion into non-endemic areas of Pakistan; a serious threat. Virol j. 2016; 13(1):144. doi: https://doi.org/10.1186/s12985-016-0603-6 [ Links ]
10. Mahmood R, Benzadid MS, Weston S, Hossain A, Ahmed T, Mitra DK, et al. Dengue outbreak 2019: clinical and laboratory profiles of dengue virus infection in Dhaka city. Heliyon. 2021; 7(6):e07183. doi: https://doi.org/10.1016/j.heliyon.2021.e07183 [ Links ]
11. Mostorino RE, Rosas AA, Gutiérrez VP, Anaya ER, Cobos MZ, García MM. Manifestaciones clínicas y distribución geográfica de los serotipos del dengue en el Perú-año 2001. Rev Peru Med Exp Salud Pública. 2022; 19(4):171-180. Disponible en: http://www.scielo.org.pe/pdf/rins/v19n4/a02v19n4.pdf [ Links ]
12. Ramos-Castañeda J, Barreto F, Martínez-Vega R, Galvão JM, Joint G, Sarti E. Dengue in Latin America: Systematic Review of Molecular Epidemiological Trends. PLoS Negl Trop Dis [internet]. 2017 [citado el 4 de julio del 2023]; 11(1): e0005224. Disponible en: https://doi.org/10.1371/journal.pntd.0005224 [ Links ]
13. Matta L, Barbosa MM, Morales-Plaza CD. Caracterización clínica de pacientes que consultaron por dengue en un hospital de tercer nivel en Cali, Colombia 2013. Biomédica. 2016; 36(1):133-139. doi: https://doi.org/10.7705/biomedica.v36i1.2627 [ Links ]
14. Wong JG, Gan VC, Ng EL, Leo YS, Chan SP, Choo R, et al. Self-reported pain intensity with the numeric reporting scale in adult dengue. PloS one. 2014; 9(5):e96514. doi: https://doi.org/10.1371/journal.pone.0096514 [ Links ]
15. Vicente CR, Lauar JC, Santos BS, Cobe VM, Cerutti CJ. Factors related to severe dengue during an epidemic in Vitória, State of Espírito Santo, Brazil, 2011. Rev Soc Bras Med Trop. 2013; 46(5):629-632. doi: https://doi.org/10.1590/0037-8682-1579-2013 [ Links ]
16. Amorim MT, Hernández LH, Naveca FG, Essashika IT, Wanzeller AL, da Silva EV, et al. Emergence of a New Strain of DENV-2 in South America: Introduction of the Cosmopolitan Genotype through the Brazilian-Peruvian Border. Trop Med Infect Dis. 2023; 8(6):325. doi: https://doi.org/10.3390/tropicalmed8060325 [ Links ]
17. Márquez S, Lee G, Gutiérrez B, Bennett S, Coloma J, Eisenberg JN, Trueba G. Phylogenetic Analysis of Transmission Dynamics of Dengue in Large and Small Population Centers, Northern Ecuador. Emerg Infect Dis. 2023; 29 (5):888-897. doi: https://doi.org/10.3201/eid2905.221226 [ Links ]
Funding: This study was funded by the project with CONTRACT No. 050-2021-FONDECYT "Metagenomics in Vectors of the Amazon Region: Identifying Potential Foci of Emerging and Re-emerging Diseases" - METAVEC.
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: July 01, 2023; Accepted: September 01, 2023











 texto en
texto en