Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.23 no.3 Lima jul./set. 2023 Epub 21-Sep-2023
http://dx.doi.org/10.25176/rfmh.v23i3.5699
Clinical Case
Uveitis - Glaucoma - Hyphema syndrome: Clinical case
1Servicio de Oftalmología, Hospital Nacional Carlos Alberto Seguín Escobedo - EsSalud. Arequipa, Perú
2Servicio de Oftalmología, Hospital III Yanahuara - EsSalud. Arequipa, Perú
3Universidad Nacional de San Agustín, Facultad de Medicina Humana. Arequipa, Perú
4Universidad Nacional Mayor de San Marcos, Facultad de Medicina Humana. Lima, Perú
5Universidad de San Martín de Porres, Facultad de Medicina Humana. Lima, Perú
Introduction:
Uveitis-glaucoma-hyphema syndrome (UGH) is a rare complication of cataract surgery, due to mechanical chafing exerted by an intraocular lens (IOL) on the iris.
Clinical case:
A 64-year-old man with a history of cataract surgery, who presented decreased visual acuity and pain in the right eye. The ophthalmological examination revealed signs of anterior uveitis, elevated intraocular pressure (IOP), microhyphema, and a single-piece foldable IOL in the sulcus that caused a mechanical chafing with the posterior face of the iris. The medical treatment was insufficient; for this reason, a folding simple-piece IOL explant surgery was performed and replaced by a three-piece IOL. Postoperative evolution was favorable.
Conclusion:
Should be suspected this complication in patients with a history of cataract surgery, especially in cases in which the IOL is in single-piece and has been implanted outside the capsular bag.
Keywords: Uveitis-glaucoma-hyphema syndrome; intraocular lens; sulcus; capsular bag
INTRODUCTION
Uveitis-glaucoma-hyphema syndrome (UGH or Ellingson syndrome) is a rare complication of cataract surgery, which occurs due to mechanical friction exerted by the intraocular lens (IOL) on the uveal tissue (iris or ciliary body) or structures of the iridocorneal angle and can occur in patients with IOL in the anterior chamber, sulcus or capsular bag. This gives rise to a broad spectrum of clinical pictures ranging from simple iris defects to transillumination, to pigment dispersion, uveitis, microhyphema or hyphema, vitreous hemorrhage, and cystoid macular edema. Intraocular pressure (IOP) may rise after disease onset or after some recurrences. Recurrent attacks of elevated IOP may result in glaucomatous damage to the optic nerve1-3.
In recent decades, IOL design and manufacturing improvements have been achieved, and new IOL placement techniques have emerged. Currently, the vast majority of IOLs are implanted in the capsular bag, which minimizes the possibility of IOLs coming into contact with uveal tissue and reduces the incidence of UGH Syndrome4,5.
Complete history taking and slit-lamp biomicroscopic examination are the key to the diagnosis of this syndrome; however, other complementary tests such as anterior segment optical coherence tomography (AS-OCT) and ultrasonic biomicroscopy (UBM) are helpful to confirm the position of the IOL6,7.
Topical treatment with corticosteroids and hypotensive drugs can help control inflammation and IOP in the short-medium term. Avoidance of parasympathomimetics is recommended due to their possible miotic effects and increased iris rubbing with the IOL. If hyphema is present, limiting physical activity, keeping the head elevated and using cycloplegic eye drops to reduce ciliary spasm will be advisable. The indication for definitive surgical treatment should be considered if vision is reduced, elevated intraocular pressure and inflammation cannot be controlled, or if progressive glaucomatous atrophy is demonstrated. If surgical treatment is required, its approach will depend mainly on the type of IOL and its location1,5,).
The case of this study is that of a patient with UGH syndrome, in which the probable pathogenic mechanism that produced it, the clinical manifestations, complementary tests and the treatment carried out for its resolution are described.
CLINICAL CASE
A 64-year-old man reported decreased visual acuity and pain in the right eye (RE) for approximately five weeks. As an important ophthalmological history, he underwent phacoemulsification surgery with IOL implantation in the RE two years ago. In the ophthalmological examination, a visual acuity of 20/200 is shown in the RE and 20/30 in the LE. The IOP was 36 mmHg and 15 mmHg, respectively. Slit-lamp examination showed mild corneal edema, with the presence of medium keratic precipitates in the lower 1/3 of the corneal endothelium, Tyndall (1+) and Flare (1+), defect in the iris on transillumination at hours 9 and 11, mild conjunctival hyperemia (figure 1a), after pharmacological mydriasis it was possible to show an IOL with a folding piece located in the sulcus with an intact posterior capsule; the left eye did not present alterations (figure 1b).
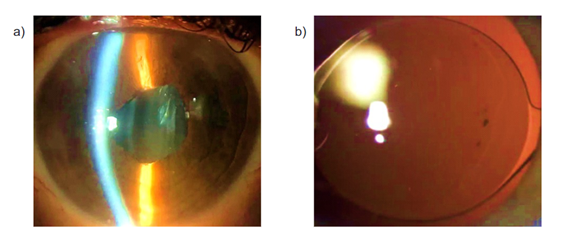
Figure 1 Right eye anterior segment biomicroscopy a) Presence of fine keratic precipitates, iris defects on transillumination at 9 and 11 hours. b) IOL of a folding piece located in the sulcus (source: Clinical report).
In the eye fundus examination, a papillary excavation of 0.4 was evidenced, without signs of inflammation in the posterior segment of the RE; in the LE, no alterations were evidenced. In RE ultrasonic biomicroscopy (UBM) performed with a 50 MHz probe, an IOL of a foldable piece can be seen displaced forward and making direct contact with the posterior face of the iris (Figure 2a); In other images, the IOL of a folding piece in the sulcus is evident, which blocks the pupil, the root of the iris is angled by the haptic of the IOL of a folding piece, in addition to the presence of Elschnig's pearls, which represent cortical remnants (Figure 2b).
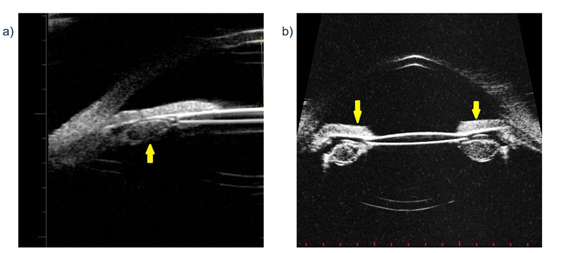
Figure 2: Ultrasonic biomicroscopy (UBM) of the right eye: a) IOL of a foldable piece making contact with the posterior face of the iris. b) IOL with a foldable piece in the sulcus, blocking the pupil (source: clinical report)
Therefore, the diagnosis of uveitis-glaucoma-hyphema (UGH) syndrome was made, and topical medical treatment was started with Brimonidine 0.2%, Dorzolamide 2%, Timolol 0.5% and Prednisolone 1% in the RE. It is reassessed at 72 hours, without evidence of clinical improvement. Because of this, surgery was planned to explant the 1-fold IOL and replace it with a 3-fold IOL, which is implanted in the sulcus (Figure 3).

Figure 3 Right eye IOL replacement surgery. One-piece foldable IOL explant and three-piece foldable IOL implant in sulcus (Source: Clinical record)
In the postoperative period, IOP remained within normal ranges, without any topical antihypertensive medication. Six weeks after surgery, visual acuity of 20/30 was obtained without correctors, an IOP of 10 mmHg, absence of inflammatory signs in the anterior segment, and clinical resolution of ocular symptoms in the RE.
DISCUSSION
Uveitis-glaucoma-hyphema (UGH) syndrome is a rare but potentially severe complication of cataract surgery. Mechanical disruption of the uveal tissues leads to dispersion of pigment, microhyphema, and release of leukocytes and proteins in the anterior chamber, and produces an inflammatory reaction. Blockage of the trabecular meshwork by debris increases intraocular pressure, causing glaucomatous changes, as occurred in the present case9.
The classic triad of UGH syndrome usually does not present in its entirety; In the present case, the UGH syndrome was secondary to the implantation of a one- piece IOL in the sulcus, which triggered the inflammatory reaction and increased IOP, without significant hyphema, which manifested with episodes of ocular pain and decreased visual acuity in the RE.
Studies have shown a higher incidence of UGH syndrome in anterior chamber (AC) lenses and those with iris fixation. However, cases associated with posterior chamber (PC) lenses have also been described. In cataract surgery, the ideal location to implant the IOL is in the capsular bag. Alternatively, some IOLs can be implanted or sutured in the sulcus and others can be placed in the anterior chamber, always keeping in mind a minimum depth of the chamber to avoid corneal decompensation due to endothelial damage10.
IOLs with a posterior chamber design, and especially one-piece ones, should be placed in the capsular bag. The three-piece IOL design would fit well into the sulcus, but require a large incision, while one-piece acrylic lenses allow for the use of smaller incisions. Nevertheless, the large haptics of one-piece IOLs do not provide a good fit in the sulcus and this location should be avoided11.
The implantation of an IOL with a foldable piece in the sulcus has a high risk of causing UGH syndrome due to traumatic rubbing of the IOL with the posterior face of the iris, as occurred in the present case. The one-piece collapsible IOL had to be implanted in the capsular bag when the phacoemulsification surgery was performed.
The traditional and definitive treatment of UGH syndrome is an explantation of the IOL, with or without reimplantation. However, in some mild cases, medical management of inflammation, hyphema, and elevated IOP is possible. Common agents include topical corticosteroids to treat inflammation, cycloplegics to prevent traumatic rubbing of the iris, prostaglandin analogs, beta-adrenergic antagonists, and alpha-adrenergic agonists to treat elevated IOP. Another medical treatment used is intracameral and intravitreal Bevacizumab for a patient with iris neovascularization and recurrent visual disturbances related to a case of "inoperable" UGH syndrome12.
In the case of requiring surgical treatment, the approach will depend mainly on the type of IOL and its location. In the case of a one-piece IOL located in the sulcus, the main indication will be to replace it with a three-piece IOL, in such a way that iris rubbing will be reduced, due to the smaller size of the haptics and because it has a rounded edge13.
In the present case, it was decided to start with topical and oral medical treatment. Subsequently, due to a minimal improvement in the clinical picture, it was decided to perform a one-piece folding IOL explant surgery and replace it with a three-fold IOL implanted in the sulcus. Later, a favorable evolution of the clinical picture was evidenced with complete resolution of the ocular symptoms in the RE.
CONCLUSIONS
Uveitis-glaucoma-hyphema (UGH) syndrome is a complication of cataract surgery whose incidence has been decreasing over the years due to the improvement in surgical techniques and further development in the design of IOLs. This clinical entity should be suspected in patients with inflammatory signs in the anterior segment, elevated IOP, hyphema/micro hyphema, and a history of cataract surgery, especially in cases in which the IOL is one-piece and has been implanted outside the capsular bag. The implantation of an IOL with a folding piece in the sulcus has a high risk of causing UGH syndrome due to traumatic rubbing of the IOL with the posterior face of the iris; as it did not respond to medical treatment, definitive surgical treatment should be considered, such as explantation of the one-piece IOL and secondary implantation of the three-piece foldable IOL in the sulcus, as occurred in the present case.
REFERENCES
1. Accorinti M, Saturno M, Paroli M, et al. Uveitis-Glaucoma-Hyphema Syndrome: Clinical Features and Differential Diagnosis. Ocul Inmunol Inflamm. 2021;1:1-6. https://doi.org/10.1080/09273948.2021.1881563 [ Links ]
2. Yang J, Qiu X, Cai L, et al. Uveitis-glaucoma-hyphema syndrome associated with an in-the-bag square-edge intraocular lens. Precis Clin Med. 2019;2(4):283-287. https://doi.org/10.1093/pcmedi/pbz026 [ Links ]
3. Mammo D, Page M, Olson J. Yoga-induced uveitis glaucoma hyphema syndrome. Digit J Ophthalmol. 2020:26(4):46-48. DOI: 10.5693/djo.02.2020.11.001 [ Links ]
4. Du Y, Zhu X, Yang J, et al. Uveitis-glaucoma-hyphema syndrome with sclera-fixed posterior-chamber two-haptic intraocular lens in a highly myopic eye: a case report. BMC Ophthalmol. 2020;20(22):1-5. https://doi.org/10.1186/s12886-020-1309-5 [ Links ]
5. Zemba M, Camburu G. Uveitis-Glaucoma-Hyphaema Syndrome. General review. Rom J Ophthalmol. 2017;61(1):11-17. DOI: 10.22336/rjo.2017.3 [ Links ]
6. Alfaro A, Vital C, Sanchez J, et al. Uveitis-glaucoma-hyphaema syndrome associated with recurrent vitreous hemorrhage. Arch Soc Esp Oftalmol. 2015;90:392-394. DOI: 10.1016/j.oftale.2015.08.007 [ Links ]
7. Piette S, Canlas O, Tran H, et al. Ultrasound biomicroscopy in uveitis-glaucoma- hyphema syndrome. Am J Ophthalmol. 2002;133(6):839-841. DOI: 10.1016/s0002-9394(02)01386-7 [ Links ]
8. Smith T, Cheung A, Hart J, Chen C. Uveitis, glaucoma, hyphema syndrome: A referral-based, retrospective analysis. Investig Ophthalmol Vis Sci. 2016;57(12):1-10. [ Links ]
9. Nath S, Rai A. Uveitis-glaucoma-hyphema syndrome after uneventful placement of a 1-piece intraocular lens into the capsular bag. J Cataract Refract Surg. 2022;10(1):1-3. https://doi.org/10.1097/j.jcro.0000000000000064 [ Links ]
10. Singh H, Modabber M, Safran S, Ahmed l. Laser iridotomy to treat uveitis-glaucoma-hyphema syndrome secondary to reverse pupillary block in sulcus-placed intraocular lenses: Case series. J Cataract Refract Surg. 2015;41(10):2215-2223. DOI: 10.1016/j.jcrs.2015.10.057 [ Links ]
11. Zhang L, Hood C, Vrabec J, et al. Mechanisms for in-the-bag uveitis-glaucoma-hyphema syndrome. J Cataract Refract. Surg. 2014;40(3):490-492. DOI: 10.1016/j.jcrs.2013.12.002 [ Links ]
12. Le T, R Doug, Sozeri Y. Uveitis-Glaucoma-Hyphema Syndrome: a Review and Exploration of New Concepts. Curr Ophthalmol Rep. 2020;8(3):1-7. https://doi.org/10.1007/s40135-020-00233-1 [ Links ]
13. El Wardani M, Kymionis G, Salmon B, et al. Uveitis-Glaucoma-Hyphema Syndrome Treated with Haptic Amputation. Klin Monbl Augenheilkd. 2019;236(4):581-583. DOI: 10.1055/a-0829-6036 [ Links ]
8Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: May 12, 2023; Accepted: July 07, 2023











 texto en
texto en 


