Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de la Facultad de Medicina Humana
Print version ISSN 1814-5469On-line version ISSN 2308-0531
Rev. Fac. Med. Hum. vol.23 no.4 Lima Oct./Dic. 2023 Epub Nov 30, 2023
http://dx.doi.org/10.25176/rfmh.v23i4.5980
Original article
Evaluation of clinical aspects related to lower limb amputation among individuals living with type 2 diabetes mellitus in Mexico
1Facultad de Farmacia. Universidad Autónoma del Estado de Morelos. México.
2Jefatura de Servicios y Prestaciones Médicas, Instituto Mexicano del Seguro Social, Cuernavaca, Morelos. México.
3Hospital General Regional con Medicina Familiar No.1, Instituto Mexicano del Seguro Social, Morelos. México.
Introduction:
Diabetes continues to be a leading cause of disability and death in the world's population. About 25% of people with diabetes will develop an ulcer in one of their lower pelvic limbs.
Objective:
The present study evaluates the clinical aspects related to lower pelvic limb amputation in a cohort of patients with diabetes mellitus. Lazarte Echegaray Hospital during the period 2017-2020.
Methods:
Retrospective, cross-sectional study, conducted in collaboration between the Mexican Institute of Social Security and the School of Pharmacy of the Autonomous University of Morelos State, involved a review of records of patients with type 2 diabetes mellitus at the Regional General Hospital "Ignacio García Téllez". One hundred clinical and electronic records were selected based on inclusion criteria, which included age over 18 years, affiliation at the study site, diabetes evolution of at least 10 years, pharmacological treatment for diabetes and diagnosis of diabetic foot with complete healing or amputation as an outcome. Statistical analyses were performed using STATA and ethical approval was obtained.
Results:
Patients with optimal glycemic control by quantifying their fasting glucose levels (<130 mg/dl) as well as their glycated hemoglobin values (< 7%) had a lower frequency of amputations (p˂0.001; Chi2) compared to those patients without adequate glycemic control.
Conclusion:
Being male, glycosylated hemoglobin values greater than 7% and mean fasting glucose values greater than 130 mg/L were found to increase the likelihood of having a lower extremity amputation.
Keywords: diabetes; glycemic; glycated hemoglobin; pharmacotherapy; major amputation; minor amputation. (Source: MESH-NLM)
INTRODUCTION
Diabetes is a major global public health concern due to its high incidence and mortality rates. In Latin America, approximately 422 million people are affected by this disease1,2. This represents a significant challenge for healthcare systems worldwide and individuals grappling with this degenerative disease3. The International Diabetes Federation (IDF) reported that in 2021, 6.7 million people worldwide succumbed to diabetes-related complications, representing 12.2% of total global deaths4. Among the health complications of diabetes, ulcerative lesions in the lower pelvic limbs are one of the most observed. The risk of amputation in people living with diabetes is 15 to 40-fold higher compared to people without diabetes5. The ulcerative lesions manifest itself in up to 25% of patients living with diabetes6, with recurrence rates of 65% at 3-5 years, leading to major and minor amputations in 20% of the cases(7). In Mexico, medical information on the prevalence and incidence of diabetic foot, amputations and the clinical aspects related to this surgical treatment is limited. However, the Mexican Institute of Social Security (IMSS) reported in 2004 an amputation rate of 169 per-100,000 patients living with diabetes, in 2013 the rate was 163 per-100,000 patients. They presented an average age of 61.7 years for major amputations and 65.4 years for minor amputations8. Another clinical cause of amputations is the manifestation of peripheral arterial disease. This is accelerated by direct damage to nerves and blood vessels resulting from high blood glucose levels9,10. In addition, the wound healing process is altered due to cellular factors involving vascular, immunological, neurological, inflammatory, and oxidative stress; alterations that lead to partial or total necrosis of the lower extremities by the induction of severe infections11,12. Lower pelvic limb amputations occur below or above the ankle joint. People with major amputations report greater pain, decreased social function, and less independence than those with minor amputations13. It is of utmost importance to consider that amputations significantly decrease the quality of life of people with diabetes14. Therefore, it is important to consider amputation as a mortality factor following surgery15,16. Consequently, there is a growing interest in developing strategies focused on diabetes prevention within healthcare systems. Recently, the Pan American Health Organization (PAHO) highlighted the importance of implementing prevention, monitoring, and control strategies for diabetes, particularly during the recent COVID-19 health emergency3. The present study evaluates the clinical aspects related to lower pelvic limb amputation in a cohort of patients with type 2 diabetes mellitus.
METHODS
Study design
In a collaborative effort between the Mexican Institute of Social Security (IMSS) and the Faculty of Pharmacy at the Autonomous University of Morelos state, a retrospective cross-sectional study was carried out, consisting of a detailed review of clinical records from patients living with type 2 diabetes mellitus assigned to the Regional General Hospital "Ignacio García Téllez" in the Morelos Delegation.
Population and sample
The clinical records of all patients living with type 2 diabetes mellitus were analyzed by reviewing the census of patients with diabetes in the family medicine information system. Two clinical pharmacist professionals were trained by two family medicine physicians to collect the information. Subsequently, the two medical professionals conducted a thorough review of the gathered data to validate compliance with the inclusion criteria. According to the International Classification of Diseases, a total of 2021 patients with multiple complications of diabetes, including vascular and neurological complications were identified, being included a total of 100 clinical records (CR) and Electronic Clinical Records (ECR) from patients who met the following inclusion criteria: age over 18 years, have a valid affiliation at the study site, have verifiable diagnosis of Type 2 Diabetes Mellitus with documented history of diabetes for at least 10 years, receiving pharmacological treatment for diabetes, receiving medical attention in the setting of the study in the period January-May 2022, and having a verifiable diagnosis of diabetic foot with complete healing or surgical amputation as outcome. The exclusion criteria included CR of patients who had passed away before the outcomes were determined, records with fewer than 2 annual fasting blood glucose measurements, and CR from patients who had requested a transfer to a different healthcare facility.
Data processing
Once the CR and ECR were identified, we proceeded to perform further review using the family medicine service’s archives, the ECR from the hospitalization service, and the clinical records from the emergency service of the Hospital. It was collected the clinical information related to foot lesions including type of lesion presented, grade according to Wagner and Meggit17, classification, location of the lesion and presence of Charcot arthropathy. Information regarding the type of amputation, such as major or minor amputation of the lower pelvic limb, was also collected, as well as the history of pharmacotherapy used in the treatment of diabetes and diabetic foot. Other data such as age, sex, main comorbidities, and laboratory values (average glycated hemoglobin and fasting glucose levels within 6 months after the diabetic foot diagnosis) were also obtained.
Statistical analysis
The qualitative variables are presented as frequencies and percentages. For quantitative variables, the mean and standard deviation are presented. Bivariate mean comparison analyses were performed using the chi2 test and t-test. The results considered statistically significant were identified with p˂0.05. Data were collected in a database using the Microsoft Excel program. All statistical analyses were performed using STATA version 12 (Statistical software).
Ethical Considerations
The present study was approved by the Local Research Committee and the Local Ethics Committee of the Mexican Institute of Social Security, Morelos (IMSS; number: R-2021-1701-040). All data from clinical records was processed using a codification and safeguarded by the researchers. No informed consent was required since this study only used clinical records.
RESULTS
The study analyzed a total sample of 100 clinical records. Among the sample, 67% of the patients had comorbidities related to overweight and obesity, followed by systemic arterial hypertension (32%) (Table 1). It was also found that 74% of the patients with diabetic foot were male patients, while 26% were female. The average age of the population analyzed was 59 years, with an age range from 32 to 86 years. The 49% of the patients presented a total or partial amputation of the lower pelvic limbs. It was identified that 30% of the cases were submitted to a minor amputation surgical intervention while 19% underwent major amputation surgery. The right lower limb was predominantly more affected in the case of minor amputations, and 69.23% of the patients with major amputations had both lower limbs affected by diabetic foot (Table 2). The grade of the lesions was reported according to the Wagner-Meggit scale by the treating physicians We identified that 40% of the patients with diabetic foot presented grade IV lesions where there was already the presence of limited gangrene, followed by grade I lesions (28%), (Table 3).
Table 1. General Information and comorbidities of patients diagnosed with diabetic foot.
| Sex | |
| Female | Male |
| 26 (26%) | 74 (74%) |
| Mean age: 59.2 ±10.5 years | |
| Years of progression of DM2: 18.65 ±9.24 years | |
| Co-morbidities | Percentage (n= 100) |
| BMI> 25 kg/m2 | 67 |
| Obesity | 33 |
| SAH | 32 |
| CKD | 15 |
| Dyslipidemia | 7 |
| Diabetic Neuropathy | 5 |
| Diabetic Retinopathy | 4 |
DM2: Type 2 Diabetes; BMI: Body mass Index; SAH: systemic arterial hypertension; CKD: Chronic Kidney disease.
Table 2. Type of amputation and pelvic limb affected in the studied population.
| Amputation | Affected limb (frequency/percentage) | |||
| Right | Left | Both | Total | |
| Major Amputation | 5 (23.81) | 5 (33.33) | 9 (69.23) | 19 (38.78) |
| Minor amputation | 16 (76.19) | 10 (66.66) | 5 (38.46) | 30 (61.22) |
| Total | 21 (100) | 15 (100) | 13 (100) | 49 (100) |
Table 3. Diabetic foot lesions according to the Wagner and Meggit classification in the studied population.
| Wagner Grade | Frequency (Percentage) | Sex | |
| Male | Female | ||
| I | 28 (28) | 15 (15) | 13 (13) |
| II | 11 (11) | 9 (9) | 2 (2) |
| III | 6 (6) | 5 (5) | 1 (1) |
| IV | 40 (40) | 31 (31) | 9 (9) |
| V | 15 (15) | 14 (14) | 1 (1) |
| Total | 100 (100) | 74 (74) | 26 (26) |
Regarding the pharmacological management of diabetes, most patients (19%) received an insulin monotherapy regimen, followed by a combination of glyburide and metformin regimen. Meanwhile, 12% of the patients were prescribed a regimen of insulin in combination with metformin. (Figure 1).
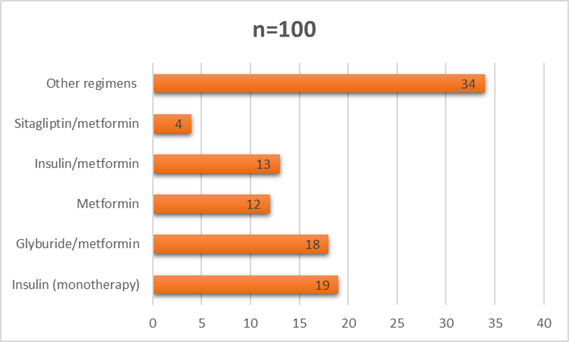
Figure 1. Main regimens of pharmacotherapy used in the treatment of diabetes in the patients included in the study.
It was performed a bivariate analysis showing that most of the patients with amputations were male, with statistically significant differences (p=0.031). Likewise, significance was identified in those patients older than 60 years of age in comparison with cases below that age (p=0.017). Amputations were also more frequent in patients with more than 10 years of diabetes evolution (p=0.001) (Table 4). The degree of average glycemic control in the six months following the diagnosis of diabetic foot was an important variable in this study. In patients with optimal glycemic control by quantifying their fasting glucose levels (less than 130 mg/dl) as well as their glycated hemoglobin values (less than 7%) according to the criteria of the Mexican Official Standard 015 for the prevention, treatment, and control of diabetes18, amputations were less frequent compared to those patients without adequate glycemic control. These biochemical parameters were statistically significant (p<0.001 and p=0.001, respectively) by Chi2test. Meanwhile, pharmacological treatments showed no relation with amputations. When evaluating the possible relationship between comorbidities, smoking, systemic arterial hypertension, obesity and being overweight (BMI> 25kg/m2), as well as Charcot arthropathy and chronic kidney disease, no statistically significant differences were found between patients with amputations and those who did not undergo such surgical procedures (Table 4).
Table 4. Bivariate analysis of amputations recorded in the study population (* Chi2).
| Variable (n=100) | Without amputation n (%) | With amputation n (%) | p* |
| Male sex | 8 (8) | 41 (41) | 0.031 |
| Over 60 years old | 32 (32) | 19 (19) | 0.017 |
| Over 10 years of diabetes evolution | 10 (10) | 39 (39) | <0.001 |
| Controlled fasting glycemia (<130 mg/dl)(18) | 19 (19) | 0(0) | <0.001 |
| Controlled glycated hemoglobin (Hb1Ac < 7%(18)) | 23 (23) | 7 (7) | 0.001 |
| History of Smoking | 13 (13) | 14 (14) | 0.729 |
| Glyburide use | 10 (10) | 15 (15) | 0.204 |
| Insulin use | 25 (25) | 25 (25) | 0.841 |
| Metformin use | 34 (33) | 33 (33) | 0.942 |
| SAH | 32 (32) | 24 (24) | 0.118 |
| BMI > 25 kg/m2 | 32 (32) | 36 (36) | 0.363 |
| CKD | 7 (7) | 7 (7) | 0.581 |
BMI: Body mass Index SAH: Systemic Arterial Hypertension CKD: Chronic Kidney disease.
DISCUSSION
In our study population we found that male patients had a higher frequency of diabetic foot (74%), as has been reported internationally19. In particular, the percentage obtained in our study was similar to that observed by Sharma21in 2016 in India (78.64%) and the reported by Vanherwegen(20)in Belgium (72%). This could be explained by considering that, as reported in the study conducted by Rangel22on a Mexican population sample in 2017, women tend to exhibit greater adherence to lifestyle changes and medication regimens which is associated with a lower risk of developing foot lesions. The mean age of patients with diabetic foot obtained in this study (59.2± 10.5 years) was very similar to that also reported by Sharma21(55.09±10.30 years), and contrasts with the reported by Vanherwegen20(69.7±0.3 years). This is mainly explained by the demographic differences in the countries in which the studies were carried out. We found an average time of evolution of diabetes of 18.65 (±9.24) years at the time of diagnosis of diabetic foot. This contrasts with that obtained by Nuñez23in Honduras in 2017, who observed an average of 10±8.0 years of time of evolution. The average age of patients with major amputation was 55.3±11.2 years, while for minor amputations, it was 59.24±11.2 years (data not shown in the tables). This is particularly relevant because the mean age for major amputations reported in 2013 by Cisneros18for the Mexican population was 61,7 years. This indicates that diabetic foot outcomes are occurring at earlier age in our study population.
Age and time of evolution of diabetes, may be related to the slow progression of vascular and neuropathic damage caused by diabetic foot ulcers, as is reported by Zhang19, who reports a longer diabetes evolution in patients with diabetic foot ulceration compared with those without a diabetic foot ulcer (11.3 ± 2.5 versus 7.4 ± 2.2 years). Our results, and those reported by Sharma and Nuñez, correspond to populations from developing countries, in which certain factors such as limited access to healthcare services, insufficient prevention programs, and medical service overload may promote the onset of diabetic foot, for instance, the limited access to clinical services. Such conditions require further exploration. The main comorbidities found in this research were overweight and obesity (BMI> 25 kg/m2) in 67% of the patients, followed by systemic arterial hypertension (32%), in contrast, Nuñez23observed peripheral vascular disease (72%) and systemic arterial hypertension (69.6%) as the main findings. It should be noted that the Mexican population exhibits one of the highest prevalence rates of overweight and obesity on a global scale. Recently, Barquera24reported an increase in the incidence of obesity of 42% between 2000 and 2018 in Mexican population.
It is also known that such metabolic conditions are related to cardiovascular diseases like systemic hypertension, which is highly spread also in the Mexican territory (prevalence of 9.6% according to ENSANUT 202125. Our study also showed that 49% of patients diagnosed with diabetic foot underwent major or minor amputation of the lower pelvic limb. This result differs from the 30.43% documented by Bekele26in Ethiopia in 2020. This difference may be explained by multiple sociodemographic and cultural differences, genetic variability between populations, and variations in the provision of health care in these territories. It is important to highlight that the 49% we observed is a remarkably high rate, undoubtedly this result suggest the limited access that certain populations have to a proper clinical follow up. It is however clear that we can expect that the population we studied was exposed to several factors that led to this outcome, the amputation of a lower pelvic limb, some of which are linked to limited pharmacotherapy access and medical assistance; non-adherence to therapy, or the lack of proper primary care policies for such vulnerable populations like the people living with diabetes. It has also been reported the barriers that may affect the proper foot care, are access to information and timely clinical appointments from health care providers27. In relation to the grade of the lesions described in this study, the results align with those identified by Ugwu28in Nigeria in 2019, where the most common lesions were grade IV according to the Wagner scale. This grade of damage implies the presence of gangrene, which increases the risk of amputation. In contrast, our findings differ from those obtained by Bekele26, who identified that 72% of cases presented lesions ranging from grade I to III, a percentage that in our study was 45%. This observation could potentially be attributed to the possibility of an early detection and therapeutic intervention in the case of these lesions, mitigating their progression towards the more severe grade IV or V categories. Regarding pharmacotherapy, most patients with diabetic foot were treated with insulin (19%). However, Navarro29in 2016 identified that the development of diabetic foot is not directly related to insulin. It is well known that adherence to insulin is usually lower compared to orally administered medications, and it is likely to worsen due to other factors such as lack of social support and especially the difficulty in measuring adequate insulin units, among others22,30. The present study found that amputations were less frequent in patients over 60 years. Possibly, due to the establishment of better conditions provided by a care giver or the provision of a therapeutic scheme that allowed long-term improvement of glycemic control; such conditions need to be further studied. Having an adequate fasting glucose level (<130 mg/dl), glycated hemoglobin levels below 7%, and being female were variables related to non-amputations. This finding is similar to the research conducted by Vatankhah31in 2016, who identified that amputations were 8.7% more frequent in those patients with higher glycated hemoglobin values. This result is also in accordance with that reported by Fan32in 2021, who reports a higher risk of amputation in males (OR:1.38, p<0.001). This study remarks the high prevalence of diabetic foot in patients with type 2 diabetes mellitus in Mexico. While results were compared with those from other countries, it is essential to consider the differences in healthcare systems, medical practices, and sociocultural factors that may influence the prevalence, management, and outcomes of the diabetic foot. These contextual disparities are crucial for gaining a better understanding of the situation in Mexico and provide significant insights into this specific population. It is noteworthy that, internationally, amputation rates have been reported to vary from as low as 3% in China to as high as 42.8% in Taiwan33, placing our study population among the higher rates of amputation. Therefore, it is recommended that future research delves more deeply into the impact of medical practices and factors related to the healthcare received by these individuals, as well as the effect of prevention policies and programs on the risk of amputation in diabetes patients. Previous evidence has demonstrated the effectiveness of these strategies in other settings34,35.
The main limitations of this study are related to the quality of the information contained in the clinical records which could have introduced biases in patient selection due to the possibility of underreporting in the diagnosis of diabetic foot. It is common for physicians to record only the presence of complications in the census, without specifying more precisely that it is diabetic foot. Additionally, deficiencies were identified in the completion of medical notes in the clinical records, as in most cases, there was a lack of detailed information on clinical characteristics and the extent of the lesions, as well as more comprehensive information on the onset of the lesions and potential risk factors identified in the physical examination. Having this data could have significantly expanded the scope of this research.
CONCLUSION
After the analysis performed in the study population, it was found that being male, having glycated hemoglobin values higher than 7% and having average fasting glucose values higher than 130 mg/L increase the probability of presenting a lower extremity amputation while other factors such as being older than 60 years and having and an optimal periodic measurement of glucose and glycated hemoglobin seem to be factors related to a lower risk.
ACKNOWLEDGMENTS
The authors recognize the valuable contribution of Zaira García Maldonado, MD, from the Mexican Institute of Social Security., and acknowledge support from the National Council of Science and Technology (CONACyT) for the PhD scholarship under the CVU 741510 and 711732 grant.
REFERENCES
1. Diabetes, Organización Panamericana de la Salud. Available from: https://www.paho.org/es/temas/diabetes ; 2022. [ Links ]
2. Herman WH. The global agenda for the prevention of type 2 diabetes. Nutr Rev. 2017; 75:13-8. [ Links ]
3. Día Mundial de la Diabetes 2020 - OPS/OMS | Organización Panamericana de la Salud. Available from: https://www.paho.org/es/campanas/dia-mundial-diabetes-2020 ; 2020. [ Links ]
4. IDF Diabetes Atlas 2021. Available from: https://diabetesatlas.org/atlas/tenth-edition/ ; 2021. [ Links ]
5. Yun JS, Cha SA, Lim TS, Lee EY, Song KH, Ahn YB, et al. Cardiovascular Autonomic Dysfunction Predicts Diabetic Foot Ulcers in Patients With Type 2 Diabetes Without Diabetic Polyneuropathy. Medicine (Baltimore). 2016;95(12):e3128. [ Links ]
6. Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med.2017; 376:2367-75. [ Links ]
7. McDermott K, Fang M, Boulton AJM, Selvin E, Hicks CW. Etiology, Epidemiology, and Disparities in the Burden of Diabetic Foot Ulcers. Diabetes Care. 2022;46(1):209-21. [ Links ]
8. Cisneros-González N, Ascencio-Montiel IJ, Libreros-Bango VN, Rodríguez-Vázquez H, Campos-Hernández Á, Dávila-Torres J, et al. Lower extremity amputation rates in diabetic patients. Rev Med Inst Mex Seguro Soc. 2016; 54:472-9. [ Links ]
9. Weledji EP, Fokam P. Treatment of the diabetic foot - to amputate or not? BMC Surg. 2014; 14:83. [ Links ]
10. Beks PJ, Mackaay AJ, de Neeling JN, de Vries H, Bouter LM, Heine RJ. Peripheral arterial disease in relation to glycaemic level in an elderly Caucasian population: the Hoorn study. Diabetologia.1995;38:86-96. [ Links ]
11. Spampinato SF, Caruso GI, De Pasquale R, Sortino MA, Merlo S. The Treatment of Impaired Wound Healing in Diabetes: Looking among Old Drugs. Pharmaceuticals (Basel). 2020;13(4):60. [ Links ]
12. Boniakowski AE, Kimball AS, Jacobs BN, Kunkel SL, Gallagher KA. Macrophage-Mediated Inflammation in Normal and Diabetic Wound Healing. J Immunol. 2017; 199:17-24. [ Links ]
13. Lu Q, Wang J, Wei X, Wang G, Xu Y.Risk Factors for Major Amputation in Diabetic Foot Ulcer Patients. Diabetes Metab Syndr Obes. 2021; 14:2019-27. [ Links ]
14. Chou YY, Hou CC, Wu CW, Huang DW, Tsai SL, Liu TH, Ding LM, Chang CK, Ou KL, Chiu YL, Tzeng YS. Risk factors that predict major amputations and amputation time intervals for hospitalised diabetic patients with foot complications. 2022.19:1329-1338 [ Links ]
15. Martínez-Escalante JE, Romero-Ibargüengoitia ME, Plata-Álvarez H, López-Betancourt G, Otero-Rodríguez R, Garza-Cantú AA, et al. Pie diabético en México: factores de riesgo para mortalidad posterior a una amputación mayor, a 5 años, en un hospital de salud pública de segundo nivel. Cirugía y cirujanos. 2021; 89:284-90. [ Links ]
16. Beyaz S, Güler ÜÖ, Bagir GS. Factors affecting lifespan following below-knee amputation in diabetic patients. Acta Orthop Traumatol Turc. 2017; 51:393-7. [ Links ]
17. Wagner FW. The dysvascular foot: a system for diagnosis and treatment. Foot Ankle.1981; 2:64-122. [ Links ]
18. Secretaría de Salud. Norma Oficial Mexicana 015 Para la prevención, tratamiento y manejo de la Diabetes. Available from: https://dof.gob.mx/nota_detalle.php?codigo=5168074&fecha=23/11/2010#gsc.tab=0 ;2010 [ Links ]
19. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Ann Med. 2017; 49:106-16. [ Links ]
20. Vanherwegen AS, Lauwers P, Lavens A, Doggen K, Dirinck E. Sex differences in diabetic foot ulcer severity and outcome in Belgium. PLOS ONE. 16 de febrero de 2023;18(2):e0281886. [ Links ]
21. Sharma R, Kapila Rajesh, Sharma Ashwani, Jagsir MAnn. Diabetic Foot Disease Incidence and Risk Factors: A Clinical Study. The Journal of Foot and Ankle Surgery 2016; 3:40-6. [ Links ]
22. Rangel YR, Suárez RM, Valdivia MG, Suárez MER, Díaz CR, Macias YC. Adherencia terapéutica en pacientes con diabetes mellitus tipo 2. Finlay. 23 2017; 7:89-98. [ Links ]
23. Nuñez D, Martinella I, Cruz R, Mourlot A. Caracterización clínico-epidemiológica de pacientes afectados por pie diabético. Rev Cub Med Mi.2017; 46:337-348. [ Links ]
24. Barquera S, Rivera JA. Obesity in Mexico: rapid epidemiological transition and food industry interference in health policies. The Lancet Diabetes & Endocrinology.2020;8:746-7. [ Links ]
25. Instituto Nacional de Salud Pública. Encuesta Nacional de Salud y Nutrición 2018. Available from: https://www.insp.mx/resources/images/stories/2022/docs/220801_Ensa21_digital_29julio.pdf ; 2021. [ Links ]
26. Bekele F, Chelkeba L. Amputation rate of diabetic foot ulcer and associated factors in diabetes mellitus patients admitted to Nekemte referral hospital, western Ethiopia: prospective observational study. Journal of Foot and Ankle Research. 2020; 13:65. [ Links ]
27. Fayfman M, Schechter MC, Amobi CN, Williams RN, Hillman JL, Alam MM, et al. Barriers to Diabetic Foot Care in a Disadvantaged Population: A Qualitative Assessment. J Diabetes Complications. 2020;34(12):107688. [ Links ]
28. Ugwu E, Adeleye O, Gezawa I, Okpe I, Enamino M, Ezeani I. Predictors of lower extremity amputation in patients with diabetic foot ulcer: findings from MEDFUN, a multi-center observational study. J Foot Ankle Res. 14 de junio de 2019; 12:34. [ Links ]
29. Navarro-Peternella FM, Lopes APAT, de Arruda GO, Teston EF, Marcon SS. Differences between genders in relation to factors associated with risk of diabetic foot in elderly persons: A cross-sectional trial. J Clin Transl Endocrinol. 2016; 6:30-6. [ Links ]
30. Leyva-Jiménez R, Rodríguez-García CA, López-Partida XM. Adherencia a la. Rev Mex Med Fam 2019; 6:7-13. [ Links ]
31. Vatankhah N, Harris SK, Wilson D, Landry G, Mitchell EL, Moneta GL, et al. PC158. Predictors of Wound Healing, Minor Amputation, and Major Amputation in Diabetic Foot Ulcers. Journal of Vascular Surgery. 2016; 63:201S. [ Links ]
32. Fan L, Wu X-J. Sex difference for the risk of amputation in diabetic patients: A systematic review and meta-analysis. PLoS ONE. 2021;16: e0243797. [ Links ]
33. Mansoor Z, Modaweb A. Predicting Amputation in Patients with Diabetic Foot Ulcers: A Systematic Review. Cureus. 2022.14(7): e27245. [ Links ]
34. Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD. Patient education for preventing diabetic foot ulceration. Cochrane Database Syst Rev. 2014. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001488.pub5/full [ Links ]
35. Singh S, Jajoo S, Shukla S, Acharya S. Educating patients of diabetes mellitus for diabetic foot care. J Fam Med Prim Care.2020;9(1):367-73. [ Links ]
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: August 19, 2023; Accepted: November 21, 2023











 text in
text in 


