Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista de la Facultad de Medicina Humana
versão impressa ISSN 1814-5469versão On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.23 no.4 Lima out./dez. 2023 Epub 30-Nov-2023
http://dx.doi.org/10.25176/rfmh.v23i4.5877
Review article
Mortality of patients hospitalized by Covid-19 in Mexico, systematic review
aFacultad de Medicina, Coordinación de Investigación, Campus Universitario Siglo XXI, Zinacantepec México
bInvestigador, Hospital para el niño del Instituto Materno Infantil del Estado de México
cInvestigador Asociado de la Universidad Anáhuac México, Centro de Investigación en Ciencias de la Salud Lomas Anáhuac 786, Huixquilucan, México
Introduction:
Since the start of the pandemic, Mexico was one of the countries with the highest mortality rates from COVID 19.
Objective:
To determine if type 2 diabetes mellitus, arterial hypertension, and obesity increase mortality in patients diagnosed with COVID-19 who required hospitalization in Mexico.
Methods:
Systematic review in Pubmed MeSH, Web of Science, Lilas, Scielo, and Google Scholar with the terms MeSH COVID-19, SARS-COV2, Coronavirus, and Mexico for the years 2020 and 2021, in English or Spanish. Two reviewers selected the studies, two additional reviewers participated in the analysis of the studies.
Results:
Seventy three studies carried out in Mexico from 2020 to 2021 were included with information obtained from the databases of the National Epidemiological Surveillance System of Mexico. With an average age of 52.9 ± 13.27 years, 64% of the included patients were women, in general, a mortality rate of 16.76% (Min-Max 0.77-73.73%) was reported. 71% of the studies (52) did not report specific mortality related to comorbidities the most prevalent pathology was obesity with 24.23% (Min-Max 11.50-71.00%), followed by arterial hypertension 22.23% (Min-Max 2.0-53.96%) and finally Diabetes mellitus with 18.10% (Min-Max 1.83-40.00%).
Conclusion:
The most common comorbidity among patients hospitalized for COVID in Mexico was obesity, followed by type 2 diabetes mellitus and hypertension.
Keywords: COVID 19; diabetes; hypertension; Mexico; mortality; obesity. (Source: MESH-NLM)
INTRODUCCIÓN
Since the WHO declared a pandemic on March 11, 2020, until December 30, 2022, a total of 7,639,825 COVID-19 cases and 345,639 deaths were confirmed, ranking fifth1in the world in terms of reported deaths.
Throughout the pandemic, sufficient evidence emerged suggesting that the severity of clinical manifestations and the disease's mortality rate vary from person to person, depending on factors such as advanced age (people over 70 years), obesity, the presence of comorbidities like diabetes mellitus, hypertension, renal disease, and diseases associated with immunosuppression and systemic inflammation2-4.
Given that in Mexico, 36.1% of adults over 20 years of age are obese5and approximately 10.32% (8,542,718) have diabetes mellitus6, during the entire pandemic Mexico remained one of the top five countries with the highest mortality rate worldwide. Hypertension, obesity, and type 2 diabetes mellitus increase the vulnerability to develop severe complications due to SARS-CoV-2 infection and are discussed below.
Systemic Arterial Hypertension
ACE2 (angiotensin-converting enzyme 2) has been recognized as the binding receptor for SARS-CoV-2 at the onset of the infectious process in a host cell. This binding is achieved through the recognition of the RBD domain belonging to the S1 subunit of the viral S protein. The distribution and presence of ACE2 in human body tissues could act as potential viral targets and, therefore, be susceptible to infection. This receptor has been highly identied in type II alveolar epithelial cells of the lung, brain, and enterocytes of the small intestine7.
ACE2 (angiotensin-converting enzyme 2) is a secreted and membrane-associated aminopeptidase expressed in various tissues8. Discovered in 2000 as a homolog of the angiotensin-converting enzyme (ACE)9, it has a potent negative regulatory action on the reninangiotensin system (RAS), which plays a signicant role in cardiovascular physiology and homeostasis through the regulation of electrolyte balance, blood pressure and vascular tone10,11. Dysfunction of the RAS results in elevated levels of angiotensin II, a vasoactive peptide with vasoconstrictive and inflammatory properties, increasing the number of macrophages and their infiltration into the vascular wall, thereby raising immune cell numbers and inammation, contributing to increased oxidative stress10.
In various animal models and human studies, it has been demonstrated that chronic administration of renin-angiotensin system (RAS) inhibitors increases the expression of ACE2. This suggests the possibility of higher susceptibility to SARS-CoV-2 infection and a more severe disease course with the use of RAS inhibitors12.
The endothelium, lining the inner wall of vessels and being the primary regulator of vascular homeostasis, modulates the balance between vasoconstriction/vasodilation, inhibits the proliferation/migration of vascular wall muscle cells, and also modulates hemostasis. Endothelial dysfunction is an event that precedes the morphological changes characteristic of atherogenesis and contributes to the development of complications of atherosclerotic plaque13.
This common denominator is most prevalent among COVID-19 comorbidities. In hypertension, sustaine delevation of systemic pressure in the microvasculature leads to premature aging and increased turnover of endothelial cells, affecting the endothelium's ability to release endothelium-derived relaxing factors, causing vasoconstriction14. Endothelial dysfunction is suggested to be involved in COVID-19 progression due to atypical manifestations among patients, such as cardiac injury and hypercoagulability, indicated by increased levels of D-dimer and Von Willebrand factor. Common inammator y markers obser ved in endothelial dysfunction, including C-reactive protein, IL-6, and TNF-alpha, are also elevated in COVID-19 patients(15). The mechanical stress caused by high intraluminal pressure in the vascular wall activates NADPH oxidase (NOX), the main enzyme producing reactive oxygen species, triggering oxidative stress leading to endothelial dysfunction. This oxidative stress incites a destructive cascade in the arterial wall followed by chronic inammation resulting in changes in the arterial wall, such as remodeling, increased intimamedia thickness, and functional remodeling16.
Obesity
Overweight and obesity are major health issues in Mexico(17). According to the latest "National Health and Nutrition Survey 2020," the combined prevalence of overweight-obesity in adults over 20 years was 76.8% in women and 73.0% in men18.
Obesity, along with other diseases like diabetes mellitus or hypertension, are risk factors and increase mortality due to COVID-19. These conditions are associated with hypertrophy and hyperplasia of adipocytes, which disrupt the balance in the production of adipokines, inducing the secretion of pro-inammatory adipokines such as leptin, interleukins (IL-1β, IL-6, and IL-8), TNF-α, MCP-1, and decreasing the production of anti-inammatory adipokines like adiponectin18,19. These cytokines cause low-grade inammation and a dysfunction of innate immunity, predisposing to the development of infections.
Leptin acts on pulmonary broblasts and contributes to lung inammation by inducing pro-inammatory cytokines and chemokines, with high leptin levels associated with more severe lung inammation in COVID-19 patients. There is a positive correlation between the duration of SARS-CoV-2 infection and the degree of interstitial brosis; pulmonary brosis due to an excess of extracellular matrix components produced by activated myobroblasts poses a barrier to gas exchange20.
The cellular receptor for SARS-CoV-2, besides being expressed in the heart, vessels, lungs, kidneys, testicles, and brain, is also present in adipose and lung tissues in obese patients21.
Elevated expression of angiotensinconverting enzyme by adipose tissue promotes greater viral replication, and adipose tissue can act as a reservoir and storage for the virus. These patients are more susceptible to thromboembolic episodes due to hypercoagulability22.
Obesity also leads to a procoagulant state, which can be exacerbated by SARSCoV-2 infection, thus leading to worse clinical outcomes23.
The function of various immune cells is also altered in obese patients; obesity affects the responses of T and B cells, thus delaying the adaptive immune response to infection. The weakened immune system in obese patients can result in a higher viral load, rapid replication, and viral spread24.
From a physiological perspective, obesity impairs respiratory mechanics and gas exchange, increases airway resistance, and reduces the strength of respiratory muscles and lung volumes25.
Type 2 Diabetes Mellitus
Diabetes is the second underlying cause of death in Mexico, accounting for 14% of deaths26,27. A metaanalysis including 33 studies reported a correlation between diabetes mellitus and disease severity, with more patients requiring invasive ventilation and ICU admission, leading to higher mortality in this group28.
Poor glycemic control in patients with type 2 diabetes mellitus is associated with magnesium deciency and a subacute proinammatory state, including increased circulating proinammatory cytokines and altered levels of lymphocytes, neutrophils, and macrophages compared to non-diabetic subjects29,30.
This lived experience underscores the need for prevention in the face of a future pandemic of this magnitude. Together, these observations indicate that to reduce the impact of SARS-CoV-2, a broad approach is required; interventions must address not only virus transmission but also a comprehensive assessment of a population's health status.
Therefore, the aim of this study was to determine if type 2 diabetes mellitus, hypertension, and obesity increase mortality in patients diagnosed with COVID-19 in Mexico
METHODS
Search Strategy
A systematic review was conducted in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) guidelines of articles published from January 2020 to December 31, 2021 in English or Spanish.
The systematic search was performed in the following databases using Boolean operators: PubMed MeSH (Medical Subject Heading) ("COVID-19"[MeSH] or "Mexico"[MeSH]) or ("diabetes mellitus" [MeSH] or "obesity" [MeSH] or "Hypertension"[MeSH] or "Mortality"[MeSH]), Scopus (Mexico and COVID-19 or CORONAVIRUS or SARS-CoV-2 or SARS) or (diabetes, obesity, and hypertension or mortality or comorbidity), Web of Science Mexico (title) and COVID-19 (all elds) and (diabetes or hypertension or obesity or mortality (all elds) and comorbidities), Lilas (Mexico and (COVID-19 or SARS-CoV-2 or Coronavirus)), Google Scholar (Mexico and (COVID-19 or SARS-CoV-2 or Coronavirus)), and Scielo (Mexico and (COVID-19 or SARS-CoV-2 or Coronavirus)). The MeSH terms used were: "review" or "literature review" or "Meta-Analysis", type of publication].
Studies without an abstract or full text were excluded. When an abstract met the inclusion criteria, which included hospitalized patients over 20 years old, with reports of the three comorbidities studied (obesity, hypertension, and diabetes mellitus) as well as mortality, the full text was reviewed. All selected articles were identied and reviewed by four authors (AP, LC, AS, SR).
Data Collection and Analysis
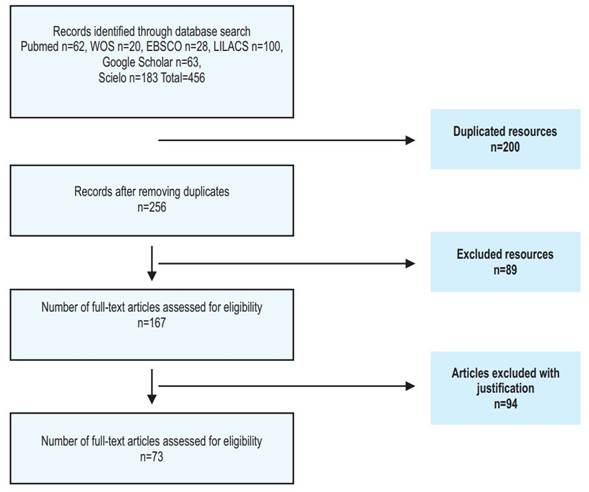
Data extraction and management were performed by two independent reviewers (AP, LC). To assess whether studies met the inclusion criteria, two additional reviewers were involved in analyzing the studies (AS, SR). The study selection process is presented in Figure 1. The information extracted and analyzed from the collected studies included the year of study, number of cases included, number of diabetic patients, number of hypertensive patients, number of obese patients, and number of deceased patients. Results are summarized narratively in each relevant section within the text of this review.
From the collected studies, the following information was extracted and analyzed: year of study, number of cases included, number of diabetic patients, number of hypertensive patients, number of obese patients and number of deceased patients..
The results are summarized narratively in each relevant section within the text of this review.
RESULTS
After searching the databases, a total of 456 studies were found. 200 duplicate records were removed, and 89 articles were excluded for not meeting selection criteria upon full article review. In a second review, two independent reviewers excluded some articles for presenting incomplete results or being studies on the pediatric population. Finally, 73 studies were included for analysis.
Characteristics of the Included Studies
The 73 included studies were conducted in Mexico, between 2020 and 2021. Most obtained information from national databases like the National Epidemiological Surveillance System with 24 studies (32.8%), and local databases like those of the National Institute of Respiratory Diseases with 20 studies (27.3%), the Ministry of Health with 19 studies (26%), and the Mexican Institute of Social Security with 10 studies (13.6%). 64% of the study population were women, with a median age of 52.9 years SD ±13.27.
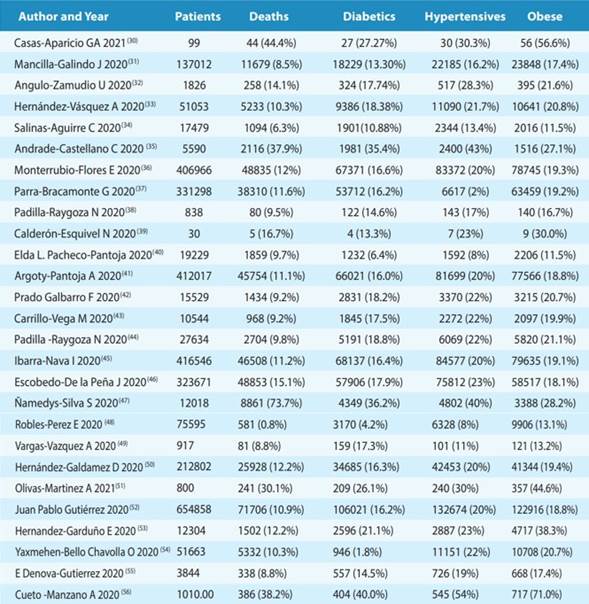
The characteristics of the studies are presented in Table 1. Generally, a mortality rate of 16.76% (Min-Max 0.77-73.73%) was reported. 71% of the studies (n=52) did not report specic mortality related to comorbidities. The most prevalent pathology was obesity with a rate of 24.23% (Min-Max 11.50-71.00%), followed by hypertension 22.23% (Min-Max 2.0-53.96%), and nally diabetes mellitus with 18.10% (Min-Max 1.83-40.00%).
DISCUSSION
The global spread of Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2) triggered an economic and health crisis worldwide.
Since the beginning of the pandemic, Mexico ranked among the top 5 countries in morbimortality, as severe COVID-19 disproportionately affects people over 70 and patients with comorbidities such as obesity, diabetes, hypertension, cardiovascular disease, chronic kidney disease, and chronic lung disease1,5, prevalent in Mexico.
The pandemic highlighted a high prevalence of undiagnosed type 2 diabetes mellitus, showing a higher risk of mortality than previously diagnosed cases. Patients with overweight/obesity and COVID-19 required more ICU admissions due to a greater need for intubation, longer hospital stays, and exhibited higher mortality compared to individuals with a BMI between 18.5 and 25 kg/m². Hospital saturation and long care times also led to increased mortality23,25.
Other factors inuencing these outcomes include Mexico's large population, with approximately 42% living in poverty5, lacking easy access to health institutions.
50% of the Mexican population is not affiliated with Social Security, relying on state or federal health services or expensive private services31. This health inequality due to poverty may be linked to a¿ higher risk of dying from COVID-19. Social vulnerability played a decisive role, as isolated communities lack adequate access to the health system32.
Mexico had one of the lowest COVID-19 diagnostic test rates per capita in the world (about 17 tests per 1000 people)33.
The pandemic management by health authorities faced criticism, with initial controversy over mask use and open international borders, which might have contributed to case numbers but not consistently to mortality.
The SARS-CoV-2 vaccination campaign in Mexico started in December 2020, targeting healthcare workers and older adults, with 63% of the population immunized by late 2021. This resulted in a reduction in severe and hospitalized COVID-19 cases, but an increase in mortality probability among hospitalized patients, mainly unvaccinated individuals34.
CONCLUSIONS
Age, gender, and comorbidities such as diabetes, obesity, and hypertension were the most frequently associated risk factors for death from COVID-19.
Demographic differences, comorbidity prevalence, healthcare capacity, and effectiveness of risk mitigation measures impact mortality and complications from COVID-19.
The Mexican health system's efforts should focus on promoting healthy lifestyles to achieve better metabolic control in diabetic and hypertensive patients, as an association between glycemic dysregulation and the severity of respiratory disease caused by SARS-CoV-2 was documented.
REFERENCES
1. World Health Organization. Archived: WHO Timeline - COVID-19 [Internet]. Wold Health Organization. 2020 [citado el 11 de junio de 2023]. p. 2020. Disponible en: https://www.who.int/news/item/27-04-2020-who-timeline---covid-19 [ Links ]
2. Noyola DE, Hermosillo-Arredondo N, Ramírez-Juárez C, Werge-Sánchez A. Association between obesity and diabetes prevalence and COVID-19 mortality in Mexico: an ecological study. J Infect Dev Ctries. 2021;15(10):1396-403. doi: 10.3855/JIDC.15075 [ Links ]
3. Stokes EK, Zambrano LD, Anderson KN, Marder EP, Raz KM, El Burai Felix S, et al. Coronavirus Disease 2019 Case Surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759-65. doi: 10.15585/MMWR.MM6924E2 [ Links ]
4. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-62. doi: 10.1016/S0140-6736(20)30566-3 [ Links ]
5. Gobierno de México. Exceso de mortalidad en México COVID-19 [Internet]. 21 de junio. 2021 [citado el 11 de junio de 2023]. Disponible en: https://coronavirus.gob.mx/exceso-de-mortalidad-en-mexico/ [ Links ]
6. INEGI. Prevalencia de Obesidad, Hipertensión y Diabetes para los Municipios de México 2018. 2020. [ Links ]
7. Radzikowska U, Ding M, Tan G, Zhakparov D, Peng Y, Wawrzyniak P, et al. Distribution of ACE2, CD147, CD26, and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors. Allergy. 2020;75(11):2829-45. doi: 10.1111/ALL.14429 [ Links ]
8. Jia HP, Look DC, Shi L, Hickey M, Pewe L, Netland J, et al. ACE2 Receptor Expression and Severe Acute Respiratory Syndrome Coronavirus Infection Depend on Differentiation of Human Airway Epithelia. J Virol. 2005;79(23):14614-21. doi: 10.1128/jvi.79.23.14614-14621.2005 [ Links ]
9. Harmer D, Gilbert M, Borman R, Clark KL. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532(1-2):107-10. doi: 10.1016/S0014-5793(02)03640-2 [ Links ]
10. Verma A, Xu K, Du T, Zhu P, Liang Z, Liao S, et al. Expression of Human ACE2 in Lactobacillus and Beneficial Effects in Diabetic Retinopathy in Mice. Mol Ther Methods Clin Dev. 2019;14:161-70. doi: 10.1016/J.OMTM.2019.06.007 [ Links ]
11. Li Y, Zhou W, Yang L, You R. Physiological and pathological regulation of ACE2, the SARS-CoV-2 receptor. Pharmacol Res [Internet]. 2020 [citado el 12 de junio de 2023];157. doi: 10.1016/J.PHRS.2020.104833 [ Links ]
12. López-Otero D, López-Pais J, Cacho-Antonio CE, Antúnez-Muiños PJ, González-Ferrero T, Pérez-Poza M, et al. Impact of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers on COVID-19 in a western population. CARDIOVID registry. Rev Esp Cardiol. 2021;74(2):175-82. doi: 10.1016/j.recesp.2020.05.030 [ Links ]
13. Carvajal C. El endotelio: estructura, función y disfunción endotelial. Medicina Legal de Costa Rica. 2017;34(2):90-100. [ Links ]
14. Xu S wen, Ilyas I, Weng J ping. Endothelial dysfunction in COVID-19: an overview of evidence, biomarkers, mechanisms and potential therapies. Acta Pharmacol Sin. 2022;44(4):695-709. doi: 10.1038/s41401-022-00998-0 [ Links ]
15. Faraj SS, Jalal PJ. IL1ß, IL-6, and TNF-a cytokines cooperate to modulate a complicated medical condition among COVID-19 patients: case-control study. Ann Med Surg (Lond). 2023;85(6):2291-7. doi: 10.1097/MS9.0000000000000679 [ Links ]
16. Chernyak B V., Popova EN, Prikhodko AS, Grebenchikov OA, Zinovkina LA, Zinovkin RA. COVID-19 and Oxidative Stress. Biochemistry (Mosc). 2020;85(12):1543. doi: 10.1134/S0006297920120068 [ Links ]
17. Barquera S, Rivera JA. Obesity in Mexico: rapid epidemiological transition and food industry interference in health policies. Lancet Diabetes Endocrinol. 2020;8(9):746-7. doi: 10.1016/S2213-8587(20)30269-2 [ Links ]
18. Shamah-Levy T, Romero-Martínez M, Barrientos-Gutiérrez T, Cuevas-Nasu L, Bautista-Arredondo S, Colchero MA, Gaona- Pineda EB, Lazcano-Ponce E, Martínez-Barnetche J, Alpuche-Arana C R-DJ. Encuesta Nacional de Salud y Nutrición 2020 sobre Covid-19 [Internet]. Cuernavaca, México; 2021. Disponible en: https://www.insp.mx/resources/images/stories/2023/docs/230811_Ensanut2020sobreCovid_Nacionales.pdf [ Links ]
19. Dafallah Albashir AA. The potential impacts of obesity on COVID-19. Clin Med (Lond). 2020;20(4):E109-13. doi: 10.7861/CLINMED.2020-0239 [ Links ]
20. Ellulu MS, Patimah I, Khaza'ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017;13(4):851. doi: 10.5114/AOMS.2016.58928 [ Links ]
21. Ni YN, Luo J, Yu H, Wang YW, Hu YH, Liu D, et al. Can body mass index predict clinical outcomes for patients with acute lung injury/acute respiratory distress syndrome? A meta-analysis. Crit Care. 2017;21(1). doi: 10.1186/S13054-017-1615-3 [ Links ]
22. Jayarangaiah A, Kariyanna PT, Chen X, Jayarangaiah A, Kumar A. COVID-19-Associated Coagulopathy: An Exacerbated Immunothrombosis Response. Clin Appl Thromb Hemost. 2020;26. doi: 10.1177/1076029620943293 [ Links ]
23. Pettit NN, MacKenzie EL, Ridgway JP, Pursell K, Ash D, Patel B, et al. Obesity is Associated with Increased Risk for Mortality Among Hospitalized Patients with COVID-19. Obesity (Silver Spring) [Internet]. 2020 [citado el 27 de junio de 2023];28(10):1806. doi: 10.1002/OBY.22941 [ Links ]
24. Kuperberg SJ, Navetta-Modrov B. The Role of Obesity in the Immunopathogenesis of COVID-19 Respiratory Disease and Critical Illness. Am J Respir Cell Mol Biol. 2021;65(1):113-21. doi: 10.1165/RCMB.2020-0236TR/SUPPL_FILE/DISCLOSURES.PDF [ Links ]
25. Biscarini S, Colaneri M, Ludovisi S, Seminari E, Pieri TC, Valsecchi P, et al. The obesity paradox: Analysis from the SMAtteo COvid-19 REgistry (SMACORE) cohort. Nutrition, Metabolism, and Cardiovascular Diseases [Internet]. 2020 [citado el 27 de junio de 2023];30(11):1920. doi: 10.1016/J.NUMECD.2020.07.047 [ Links ]
26. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4-14. doi: 10.1016/J.DIABRES.2009.10.007 [ Links ]
27. INEGI. Comunicado de prensa 538/19. Características de las defunciones registradas. 2019;1-65. [ Links ]
28. Kumar A, Arora A, Sharma P, Anikhindi SA, Bansal N, Singla V, et al. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes and Metabolic Syndrome: Clinical Research and Reviews. 2020;14(4):535-45. doi: 10.1016/j.dsx.2020.04.044 [ Links ]
29. Alegre-Díaz J, Herrington W, López-Cervantes M, Gnatiuc L, Ramirez R, Hill M, et al. Diabetes and Cause-Specific Mortality in Mexico City. New England Journal of Medicine [Internet]. 2016 [citado el 27 de junio de 2023];375(20):1961-71. doi: 10.1056/NEJMOA1605368/SUPPL_FILE/NEJMOA1605368_DISCLOSURES.PDF [ Links ]
30. Bradley SA, Banach M, Alvarado N, Smokovski I, Bhaskar SMM. Prevalence and impact of diabetes in hospitalized COVID-19 patients: A systematic review and meta-analysis. J Diabetes [Internet]. 2022 [citado el 13 de agosto de 2023];14(2):144-57. doi: 10.1111/1753-0407.13243 [ Links ]
31. Juárez-Ramírez C, Reyes-Morales H, Gutiérrez-Alba G, Reartes-Peñafiel DL, Flores-Hernández S, Muños-Hernández JA, et al. Local health systems resilience in managing the COVID-19 pandemic: lessons from Mexico. Health Policy Plan [Internet]. 2022 [citado el 16 de septiembre de 2023];37(10):1278-94. doi: 10.1093/HEAPOL/CZAC055 [ Links ]
32. Juárez-Ramírez C, Théodore FL, Gómez-Dantés H. Vulnerability and risk: reflections on the COVID-19 pandemic. Rev Esc Enferm. 2022; doi: 10.1590/S1980-220X2020045203777.Vulnerability [ Links ]
33. Villafuerte-García A. La detección del SARS-CoV-2: un elemento crítico para el control de la pandemia. Facultad de Medicina UNAM. 2022;3(27):8-12. [ Links ]
34. Parra-Bracamonte GM, Lopez-Villalobos N, Velazquez MA, Parra-Bracamonte FE, Perales-Torres AL, Juárez Rendón KJ. Comparative analysis of risk factors for COVID-19 mortality before, during and after the vaccination programme in Mexico. Public Health. 2023;215:94-9. doi: 10.1016/J.PUHE.2022.12.006 [ Links ]
Article published by the Journal of the faculty of Human Medicine of the Ricardo Palma University. It is an open access article, distributed under the terms of the Creatvie Commons license: Creative Commons Attribution 4.0 International, CC BY 4.0 (https://creativecommons.org/licenses/by/1.0/), that allows non-commercial use, distribution and reproduction in any medium, provided that the original work is duly cited. For commercial use, please contact revista.medicina@urp.edu.pe.
Received: August 18, 2023; Accepted: December 05, 2023











 texto em
texto em