Introduction
ST elevated myocardial infarction (STEMI) is a frequent cause of mortality and morbidity worldwide, and among its causes, some abnormalities of the coronary arteries, such as coronary ectasia (CE), are reported in up to 3% of cases 1,2.
It is assumed that myocardial infarction in patients with CE is more frequent than in patients without CE (26.8% vs. 19.1%) 3, and in one-third of CE cases that are discovered during acute coronary syndrome, the infarct-related artery (IRA) had CE 4.
Some data link the origin of CE to alterations in nitric oxide (NO) function, inflammation, and damage to the coronary collagen matrix 5. It is also known that people living at high altitudes have overexpression of NO, endothelial damage, and products that can alter the proper function of coronary arteries 6. Observations from daily practice in the study center have found more cases of CE in patients with STEMI who are referred from high-altitude places to the hospital for reperfusion treatment.
To date, no direct association has been described in the literature between chronic exposure to high altitudes and the development of CE complicated with STEMI. Given that a significant percentage of the population in our country lives in high-altitude cities and that cardiovascular disease represents the second leading cause of death (especially of ischemic etiology), the objective of this study is to evaluate the association between chronic exposure to an altitude above 2500 meters above sea level (masl) and the presence of CE in patients with STEMI.
Materials and methods
Design and population
A matched case-control study was conducted, matching cases and controls by age and sex, using the myocardial infarction database of the study center. It included patients older than 18 years with STEMI treated at the National Cardiovascular Institute INCOR in Lima, Peru, between 2016 and 2022.
Cases were patients with STEMI who had CE on coronary angiography of the IRA, while controls were patients with STEMI without CE on angiography of the IRA.
Patients with a history of myocardial infarction and/or myocardial revascularization, rheumatological or chronic obstructive pulmonary disease, native from sea level or an altitude below 2500 masl regardless of the number of years lived at high altitude, native of high altitude living at sea level or below 2500 masl, medical records that did not indicate place of origin and birthplace, pregnant women, and undetermined culprit artery were excluded from the study.
Sample design
As there was no data in the literature, a pilot study was conducted to determine the proportion of patients with STEMI exposed to high altitudes during 2016 and treated in the study center. Out of 191 STEMI cases, 15 patients (7.9%) were from high-altitude cities. A sample size estimation was performed for the pilot study with a 99% confidence interval (CI), resulting in a sample size of 56 cases with STEMI. It was found that 40% of patients exposed to high altitudes and 3% of those not exposed to high altitudes had CE. This resulted in an odds ratio (OR) of 16.3 for the presence of CE in those exposed to high altitudes.
Using these data from the pilot study, the sample size calculation for a matched paired case-control study was performed. With a 95% confidence level, 80% power, a case-control ratio of 1:1, the percentage of controls exposed to high altitudes according to the pilot study (5.7%), and the percentage of cases exposed to high altitudes of 50%, a minimum sample size of 18 pairs was obtained, making a total of 36 patients with STEMI for the study.
Study variables
The dependent variable was the presence of CE in the IRA, evidenced during coronary angiography. The independent variable was chronic exposure to high altitudes, defined as the habitual residence of the patient at an altitude greater than or equal to 2500 masl. To determine whether a case or control met the criterion of chronic exposure to high altitude, data from medical history were used first (indicating the patient’s habitual residence at high altitude). Additionally, the patient’s national identification document’s location data and the presence of prior medical visits to the healthcare center in the high-altitude location were checked to corroborate these details.
Intervening variables included a history of hypertension, type 2 diabetes mellitus, dyslipidemia (a history of diagnosed hypercholesterolemia, hypertriglyceridemia, or both, or elevated LDL cholesterol and/or triglycerides values on admission to the hospital), smoking (current smoking history), and hematocrit at the time of hospital admission.
Data collection procedures and techniques
The data were obtained from the medical records of patients with STEMI treated at the study center. The images of coronary angiography for cases described as having CE were evaluated by two interventional cardiologists to determine whether the diagnosis was correct. Both cardiologists made their diagnoses individually, and a third opinion was sought in case of disagreement. Controls were randomly selected from the STEMI database of the study center and matched to the cases in a 1:1 ratio by sex and age (+/- 5 years).
Statistical analysis
Variables were expressed as frequencies and percentages for categorical variables and as the means or medians with their respective dispersion measures for continuous variables, depending on the distribution. Measures of association between categorical variables were calculated using the chi-squared test; for numerical variables, the t-test was used for normally distributed data.
Hypothesis testing was performed by determining the OR between exposure to high altitude and CE. Finally, because the case-control study was matched by age and sex, a conditional logistic regression analysis was conducted to determine the impact of other confounding variables. All statistical procedures were performed using Stata® software version 17.
Ethical considerations
The study protocol was approved by the Ethics Committee of the Universidad Peruana Cayetano Heredia and the Ethics Committee of the National Cardiovascular Institute-INCOR. As it was a retrospective study based on medical record data, informed consent was not needed. No patient-identifying data were collected, and all information was for the exclusive use of the researcher. No patient was involved in the design or conduction of this research.
Results
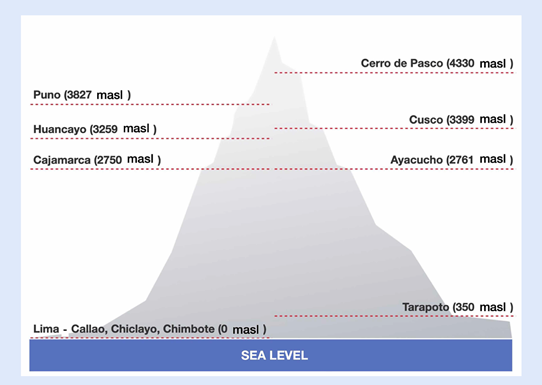
Over six years (2016-2022), 18 cases of STEMI and CE were found and were compared to 18 patients without CE. The overall average age of the population was 65 ± 9 years; 89% were males, 58% had hypertension, 22% had diabetes, 72% had dyslipidemia, and 19.4% were smokers. Thirteen patients came from high-altitude locations (36.1%), including the cities of Cusco (5 cases), Cajamarca (2 cases), Huancayo (2 cases), Puno (2 cases), Ayacucho (1 case), and Cerro de Pasco (1 case). Twenty-three patients (63.9%) came from sea-level locations (Lima, Callao, Chiclayo, Chimbote), and one patient from the city of Tarapoto (350 masl), (Figure 1).
The characteristics of the study population are presented in Table 1. Among patients exposed to high altitudes, 76.9% had CE of the IRA, while in those not exposed to high altitudes, the finding of CE was 34.7% (p=0.035).
Table 1 Clinical characteristics of cases and controls.
| Variable | Cases with CE | Controls without CE | P value |
|---|---|---|---|
| Age (years)* | 65.7 ± 9.8 | 65.5 ± 9.6 | 0.946 |
| Hematocrit* | 46.2 ± 7.3 | 42.5 ± 5.3 | 0.094 |
| Male sex | 16 (88.8%) | 16 (88.8%) | 1.000 |
| Patient from high altitude (> 2500 masl) | 10 (55.6%) | 3 (16.7%) | 0.035 |
| Hypertension | 12 (66.7%) | 9 (50%) | 0.500 |
| Diabetes mellitus type 2 | 1 (5.6%) | 7 (38.8%) | 0.041 |
| Dyslipidemia | 13 (72.2%) | 13 (72.2%) | 1.000 |
| Smoking | 5 (27.8%) | 2 (11.1%) | 0.402 |
* Mean and standard deviation
CE: Coronary Ectasia
masl: meters above sea level
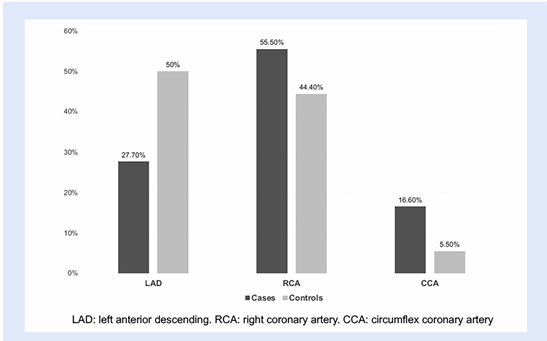
The average hematocrit was slightly higher in cases with CE than in controls, with no significant difference (46.2% versus 42.5%; p=0.094). Similarly, the average hematocrit values were higher in high-altitude natives (49.7% ± 6.6 and 41.3% ± 4.3, p=0.0001). In the CE cases, the IRA most affected was the right coronary artery (55.6%), while in controls, it was the left anterior descending artery (50%), (Figure 2).
The bivariate and multivariate conditional logistic regression analysis revealed that high-altitude residents with STEMI had six times the risk of having CE of the IRA, but this relationship was not statistically significant (Table 2).
Table 2 Bivariate and multivariate conditional logistic regression analysis.
| Variable | Bivariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| OR (CI 95%) | P value | OR (CI 95%) | P value | ||
| Patient from high altitude (> 2500 masl) | 3.3 (0.9 - 12.1) | 0.067 | 6.03 (0.30- 118) | 0.236 | |
| Hypertension | 2 (0.5 - 7.9) | 0.327 | 0.6 (0.04 - 8.1) | 0.704 | |
| Dyslipidemia | 1 (0.2 - 4.9) | 1.000 | 0.9 (0.12 - 8.1) | 0.994 | |
| Smoking | 2.5 (0.4 - 12.8) | 0.273 | 22.3 (0.7 - 667) | 0.073 | |
| Hematocrit | 1.1 (0.9-1.2) | 0.127 | 1.14 (0.9 - 1.4) | 0.290 | |
masl: meters above sea level
Discussion
In this retrospective matched case-control study of STEMI patients treated at a national reference center in Peru, no association was found between exposure to high altitudes and CE when adjusted for other risk factors, such as hypertension, dyslipidemia, smoking, and hematocrit value.
CE is a diffuse abnormal dilatation of the epicardial coronary artery greater than 1.5 times the adjacent coronary segment and exceeds more than one-third of its length, is diagnosed by coronary angiography or coronary CT angiography 7 and can be found in 2.7% of coronary angiographies, is more common in young men and coexists with coronary atherosclerotic disease in 87% of cases 8. The prevalence of CE in patients with STEMI is 3 to 3.2%, and it has been associated with major adverse events during follow-up 1,2. Furthermore, it is assumed that myocardial infarction in patients with CE is more frequent than in patients without CE (26.8% vs. 19.1%) 3, and in one-third of CE cases discovered during acute coronary syndromes, the IRA has CE 4.
CE etiopathology is related to some nitric oxide-derived products that chronically stimulate the vascular endothelium, cause coronary dysfunction, and develop CE through the activation of matrix metalloproteinases, which are enzymes that degrade the extracellular matrix of the vascular wall 5. Other clinical conditions related to CE are classic endothelial dysfunction, rheumatological diseases, Kawasaki disease, familial hypercholesterolemia, Chlamydia pneumoniae infections, cocaine addiction, sickle cell disease 5,7,9, genetic predisposition 10, elevated triglyceride levels, LDL/HDL ratio, and other known coronary risk factors (hypertension, diabetes mellitus, smoking) 11,12.
Studies in high-altitude residents (living above 2500 meters above sea level [masl]) 13 have found overexpression of NO with abnormal production of endothelial damage-related products 6. Hypobaric hypoxia, which is responsible for the development and progression of acute and chronic mountain sickness 14,15, occurs in almost 10% of the population in the Andes above 2500 masl 16 and has been linked to inflammatory and oxidative response, increasing the levels of oxidative-inflammatory-nitrosative (OXINOS), which has been associated with endothelial dysfunction and structural damage to the blood vessels 6.
In addition, other classic coronary disease risk factors could be the origin of endothelial dysfunction in this population. For instance, arterial hypertension may be higher as altitude increases (Tibetan natives) or lower as altitude increases above sea level (Andean natives) 17. Regarding dyslipidemia, there is a higher prevalence of hypertriglyceridemia and reduced HDL cholesterol in Tibetan natives, although findings are controversial and strongly associated with lifestyle and socioeconomic factors 13. For type 2 diabetes mellitus (DM2), an inverse association with altitude has been reported in males 18, and a cross-sectional study in Peru found an inverse association between altitudes above 2500 masl and the 10-year Framingham risk score, particularly in terms of the presence of diabetes mellitus 19.
Globally, approximately 81 million people live at high altitudes, representing 1.07% of the world’s population. In Peru, approximately 8 million people live above 2500 masl, constituting 25% of the Peruvian population 20. There are limited data on the prevalence of CE in Peru. A recent study found a prevalence of CE of 1.2% of total catheterizations over eight years (91 cases), with 15% of these (13 cases) associated with STEMI 21. The same authors reported a higher frequency of CE associated with acute coronary syndromes in patients from cities above 2500 masl, and the right coronary artery was the most affected coronary artery, as in this report.
Our population is similar to what Wang reported, where CE associated with STEMI was higher in males in their sixth decade of life (74% of males with an average age of 62 years) 1. While the study found that hematocrit was slightly higher in high-altitude residents, only one patient met the criteria for chronic mountain sickness (hematocrit of 63% in a patient from the city of Puno). Ninety percent of high-altitude patients had a hematocrit of less than 60%. This elevation of hematocrit could be a link between exposure to high altitudes and the development of CE, emphasizing the importance of studying other factors related to high-altitude exposure (inflammation, hyperviscosity, endothelial dysfunction, etc.) that could influence the occurrence of CE.
Despite the physiological and pathophysiological changes found in high-altitude residents, this study failed to establish a relationship between these changes and the occurrence of CE, possibly due to the study’s design (matched prevalent case-control), the small sample size, and the use of data from medical records not collected by the researcher.
The importance of further studying the relationship between CE and exposure to high altitudes lies in the potential for implementing special treatment measures for STEMI patients from high altitudes. For example, fibrinolysis (within the appropriate time frame) before invasive treatment to reduce the typical thrombotic burden in CE patients or the use of coronary thrombus aspiration as a standard measure during catheterization. While these measures could be effective, more studies are needed to demonstrate their utility in STEMI patients with CE. Currently, there are reports of increased use of thrombectomy and a lower rate of stent implantation in this context 1.
There is also controversy regarding anticoagulation in the group of postmyocardial infarction patients with CE. Multivariate analysis revealed that the risk of major cardiac events (MCE) is higher in patients with myocardial infarction due to CE (HR 4.94, 95% CI 2.36-10.4, p<0.001) during 4-year follow-up and that with appropriate anticoagulation use (warfarin with optimal time in therapeutic range >=60%), this risk of MCE significantly decreases 2. Currently, there is an ongoing study in Latin America that will attempt to determine the best anticoagulation-antiplatelet strategy for these patients 22.
The study has limitations inherent to a prevalent case-control (reporting bias) and a small sample size, which is related to the low prevalence of the disease in the population. Therefore, a definitive association between exposure to high altitudes and the presence of CE in STEMI patients cannot be ruled out, which leads to the possibility that a type II error may have occurred during the study (rejecting the alternate hypothesis when it is true).
Since this is a retrospective study, other factors related to the presence of CE mentioned in the literature (including laboratory values) were not studied due to the absence of complete data in the medical records. The results may only apply to the STEMI population because, for ease of conducting a coronary angiography (the gold standard) in these patients, this diagnostic method was chosen over coronary computed to angio-tomography for patients with chronic coronary syndrome, as it is not available in many high-altitude locations from which our patients originated.
In conclusion, in this study of STEMI patients, there was no association between chronic exposure to high altitudes and the presence of CE of the IRA. I suggest implementing a nationwide incident case-control study of CE in the entire context of coronary artery disease (stable and unstable angina and infarction) and not only in STEMI. In addition to being able to collect important data to ensure chronic exposure to high altitude (including from previous generations of the patient), relevant laboratory and clinical data could also be obtained to better characterize the association between exposure to high altitude and the development of CE.