Since the beginning of the last century, the stethoscope has been one of the most important diagnostic tools for cardiovascular evaluation and diagnosis 1. It is well known that just 50 years ago, the management of practically any condition was based on the data obtained after a complete medical history and physical examination. However, despite the physical examination continues to be a useful resource, available at the patient’s bedside and that can provide a large amount of meaningful data, in numerous settings the advent of new diagnostic modalities, especially ultrasound imaging, have demonstrated a better performance, particularly in cardiovascular physical examination 2,3.
Auscultation plays a key role in the daily work of Cardiologist for detecting evident heart abnormalities, and this pillar of the physical examination has been used as part of some of the most important classifications and scales in Cardiology, such as Killip and Kimball (KK) in the context of acute myocardial infarction (AMI), which was described for the first time in 1967, and has been validated in multiple studies and used widely so far as a prognostic tool. Stages KK I (no signs of congestion) and KK II (heart failure signs [HF], S3 sound and basal rales) have the best prognosis. On the other hand, stages KK III (acute pulmonary edema) and KK IV (cardiogenic shock) confer the worst prognosis at 30 days post-acute myocardial infarction 4,5. Stages III and IV are the most affordable to identify with auscultation. However, mainly stage II can go unnoticed by inexperienced ears.
Given this situation, lung ultrasound (LUS) has come to solve this problem by being able to evaluate pulmonary congestion more objectively. LUS is a focused technique that is fast, and harmless for the patient, and easy to reproduce for the operator and has begun to form part of the cardiologist’s tools, particularly in the emergency department 6. LUS has been validated mainly in patients with acute decompensated heart failure (ADHF). In the LUS-HF trial, it was shown that a LUS-guided diuretic treatment strategy was associated with reduced decompensations and improved walking capacity at six months of follow-up 7. In addition, in a post-hoc analysis of this study, it was demonstrated that subclinical congestion at discharge (defined as the presence of ≥5 B-lines in the LUS test in the absence of rales in the auscultation) was associated with a worse prognosis at 6-month follow-up (mainly by a higher HF admission rate in the group of patients with subclinical pulmonary congestion) with a tendency for higher rates of mortality. Interestingly, outcome rates between patients with subclinical pulmonary congestion and patients with clinical congestion (rales) at discharge were similar 8, which tells us about the great impact that subclinical congestion has on the prognosis of these patients.
In the setting of AMI, there are recent studies that have evaluated pulmonary congestion by LUS in this group of patients. For example, Araujo and co-workers 9 described that in their cohort of patients with ST elevation myocardial infarction (STEMI), 45 patients (41%) who were classified as KK I when performing LUS were classified as “wet lungs” (more than 3-b lines at least in one zone). In the same line, He et al.10, Araiza-Garaygordobil and co-workers 11, and a sub-analysis of the PARADISE-MI trial 12) described a non-negligible number of patients with STEMI that, despite having been classified as KK I had an important number of B-lines in LUS (42%, 42.8%, and 25%, respectively). However, what is the clinical importance of this discordance? Is it clinically relevant? Does it have a real impact on the prognosis of patients? The answer is yes. In all these studies, the presence of B-lines in STEMI patients increases mortality exponentially (the greater the number of B lines, the greater the mortality is) in the short (30 days) and long term (8 months), independently of the KK grade. (Figure 1).
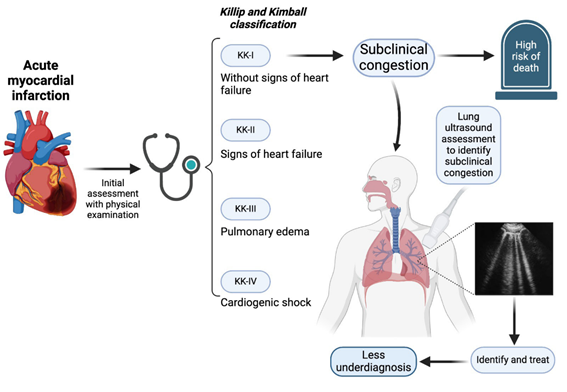
Figure 1 Utility of lung ultrasound in the context of STEMI, mainly in the identification of subclinical congestion in those patients classified as Killip and Kimball Class I.
Despite growing evidence of the great usefulness of ultrasound as an initial evaluation of STEMI patients, little is known about the clinical impact of the presence of pulmonary congestion in patients classified as KK-I at admission (theoretically there are no signs or symptoms of congestion). A Spanish group directed by Carreras-Mora 13 evaluated 312 patients with STEMI which were classified as KK-I, later dividing them into two groups, wet and dry lung, according to the number of B-lines (3 or more in at least one zone). The presence of early subclinical pulmonary congestion identified by LUS in patients with KK-I STEMI at hospital admission was associated with adverse outcomes during hospitalization and 30-day follow-up. However, it is important to note that the results were bordering.
Araujo et al.9 were the first group that developed a classification that combine clinical and LUS findings named lung ultrasound combined with KK (LUCK I: zero positive zones; LUCK II: either 1) mild B profile or 2) patients with Killip I and severe B profile; LUCK III: either 1) Killip II classification with severe B profile or 2) Killip III patients; and LUCK IV: those with clinical evidence of cardiogenic shock regardless of LUS findings; they demonstrated that LUS added to KK classification was more sensitive than physical examination only to identify patients at risk for in-hospital mortality, therefore, it is necessary to validate this classification with larger population samples, since it could be applicable in any center that has ultrasound in the Emergency Department. In agreement with this study, Dávila-Román and Checkley commented that the addition of LUS to the clinical assessment of critically ill patients provides invaluable prognostic information, coupled with the speed of obtaining it 14. Also, He et al.10) demonstrated that the addition of LUS to the KK classification provides significant incremental prognostic value, which can be an independent predictor of worsening heart failure in AMI during hospitalization and short-term follow-up.
More recently, Carreras-Mora et al.15 created a new simplified classification called “Killip pLUS”, making a comparison between their new classification and the KK and LUCK classifications. This multi-center cohort included 373 patients with the diagnosis of STEMI, and lung ultrasound was performed within the first 24 hours of admission. The authors demonstrated a better performance to predict in-hospital mortality with Killip pLUS (AUC 0.90, 95% CI 0.85-0.95) compared with KK (AUC 0.85, 95% CI 0.73-0.96) and LUCK (AUC 0.83, 95% CI 0.70-0.95). This study demonstrates that the addition of lung ultrasound provides substantial benefits when it comes to predicting worse outcomes in comparison to the exclusive use of the stethoscope.
One of the most important advantages of LUS is that, throughout multiple studies, it has been demonstrated that many hours of training are not necessary to learn how to do it properly (2 hours of reading and 10 ultrasound scans), if there is an expert to supervise, direct, and teach initially 16,17. Iminashi et al.18) addressed this aspect in patients with residual congestion due to heart failure, and they found a substantial agreement inter-operator between residents and the expert (κ = 0.86), as well as a very high (0.91) Spearman rank correlation coefficient for the B-lines between the expert and residents.
Unfortunately, ultrasound devices are not widely available, particularly in developing countries, hence physical examination continues to be of great importance. The contemporary clinic needs to be founded on the experience collected through the centuries and combine it with the technological advances. Despite this, it should not be assumed that new technologies will completely replace the usual methods, since the physical examination will always have an essential role in the decision-making 6. Quoting Dr. Ignacio Chávez: “Medicine was clinical at birth, and it will always be clinical, no matter how profound its scientific transformation. Otherwise, it wouldn’t be medicine”. However, the limitations of the clinic must be considered and know how to use the tools that are available. In this sense, particularly in STEMI, LUS should (or must) be a key tool for the cardiologist and physicians in the ED at the primary evaluation. However, more studies that evaluate subclinical congestion are required to completely establish the role of LUS in STEMI initial evaluation.















