Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.4 Lima Oct./Dic 2022 Epub Nov 30, 2022
http://dx.doi.org/10.31403/rpgo.v68i2459
Case report
Intrafetal laser therapy for twin reverse arterial perfusion sequence (TRAP). Case report and literature review
1. Physician Obstetrician and Gynecologist, Perinatology Service, San Felipe Clinic, Lima, Peru
2. Student, Facultad de Medicina Humana, Universidad Nacional Mayor de San Marcos, Lima, Peru
A 41-year-old primigravida with double monochorionic biamniotic gestation, with a diagnosis of twin reverse arterial perfusion sequence (TRAP) and poor perinatal prognosis underwent intrafetal laser surgery at 18 weeks of gestation. It was complicated with premature rupture of membranes that was managed expectantly until 33 weeks 3 days, when elective caesarean section was performed without complications. A healthy live newborn of 2,255 g was obtained and was discharged from the hospital on the 15th day of birth without complications. We report the first case of intrafetal laser surgery performed in our country and highlight its efficacy, simplicity, low cost and ambulatory approach in cases of TRAP sequence.
Key words: Pregnancy; multiple; Laser coagulation; Fetal Therapies; Ultrasonography; prenatal; Minimally invasive surgical procedures
Introduction
Twin reverse arterial perfusion (TRAP) sequence is a rare phenomenon whose incidence has been estimated at 1:35,000 pregnancies. Due to improved ultrasound diagnosis and the spread of assisted reproductive technologies in recent years, it is currently found in 1 in 9,500-11,000 pregnancies1. In this phenomenon there is a viable twin (pump) that feeds a non-viable twin (acardiac) by means of a retrograde flow through arterio-arterial and/or veno-venous anastomosis with deoxygenated blood. This peculiar circulation causes a deficit in the development of the 'acardiac' twin, in which the lower half is usually more developed due to a diversion of blood to the iliac vessels. This generates greater hemodynamic demand in its development, which can trigger congestive heart failure, fetal hydrops, premature delivery and even intrafetal death (51% risk in expectant management)2,3.
The diagnosis is made in the first trimester or at the beginning of the second trimester, being confirmed by a color Doppler study, where a retrograde blood flow pattern towards the acardiac twin is evidenced.
The presence of fetal heartbeat in the latter does not rule out the diagnosis, since according to the shape and the absence of internal organs it can be morphologically classified as 'acephalus' (without head) (60 to 75%), 'amorphus' (without shape) (20%), 'anceps' (without face) (10%) and 'acormus' (without trunk) (5%). Poor prognostic factors include hydrops, polyhydramnios, abnormal Doppler of the 'pump' twin, 'acardiac' twin/pump twin weight ratio > 70%, presence of a well-developed upper limb body in the 'acardiac' twin and monoamniotic pregnancy4.
Different therapeutic options have been described, such as interstitial laser, bipolar cord coagulation, fetoscopic laser photocoagulation of the cord, intrafetal radiofrequency ablation (RFA), among the main ones5,6. These are aimed at interrupting the intergemellar vascular circuit avoiding the increase in cardiac output of the 'pump' twin. Premature rupture of membranes (PROM), preterm delivery and intrauterine death are reported to be the main complications of intrafetal therapies. The optimal technique for treating the TRAP sequence is still a matter of debate. We report the first case of a biamniotic monochorionic twin pregnancy with TRAP sequence treated with intrafetal laser in a private center in Peru.
Case report
A 41-year-old primigravid female with double monochorionic biamniotic gestation of 12 weeks (last menstrual period 27/03/21), from Trujillo, a teacher with a history of in vitro fertilization (IVF) and arterial hypertension being treated with methyldopa was referred for consultation for presenting TRAP sequence. Ultrasonographic evaluation showed an acardiac twin/pump twin ratio of 64% (guarded prognosis) (Figure 1), so Doppler control was suggested every 2 weeks and the possibility of surgery at 16 weeks. Three weeks later (15 weeks), the control ultrasound revealed a significant increase in the 'acardiac' twin/'pump' twin ratio to 92%, so she was scheduled for intrafetal laser surgery, which was performed at 18 weeks gestation. After obtaining written consent, under local anesthesia and continuous ultrasound visualization, a 16-gauge needle was introduced into the abdomen of the acardiac fetus at the entrance of the umbilical cord, achieving photocoagulation in its intraluminal portion after 1 hour and 15 minutes, with good heart rate in the 'pump' twin and absence of flow inside the acardiac fetus (Figure 2).
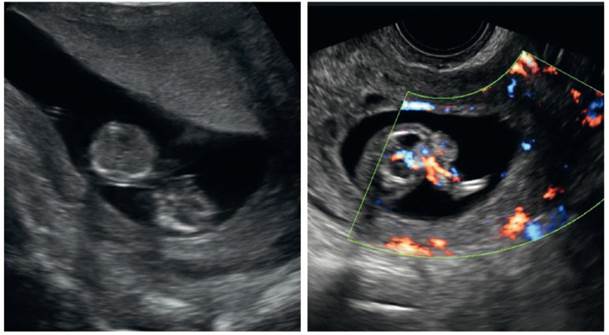
Figure 1 In the figure on the left both twins are shown, being the acardiac twin the one located in the lower part. The figure on the right shows the vascularization at the level of the umbilical cord inflow of the acardiac twin at 16 weeks.
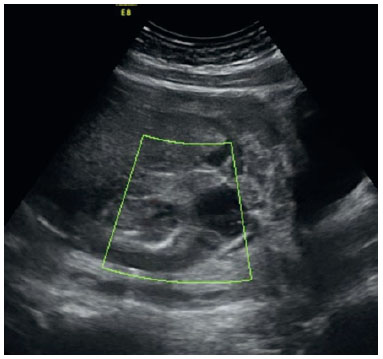
Figure 2 After the procedure performed (intrafetal laser), no Flow is observed inside the acardiac twin.
The patient went to the recovery room and after 2 hours to her room, where the obstetrics staff reported amniotic fluid leakage. The scheduled discharge was suspended and an autologous blood patch was placed transvaginally that same day. The following day, the patient remained in absolute rest and there was no amniotic fluid leakage, so she was discharged a day later. Unfortunately, upon arrival home, the patient again presented vaginal fluid leakage.
On the third postoperative day, a new ultrasound evaluation was performed, showing a maximum well of 20 mm and a fetal heart rate of 140 beats per minute. The patient did not present tachycardia, fever or abdominal pain, so it was agreed to return her to Trujillo, where she came from, for hospitalization in a local hospital. The pregnant woman remained hospitalized until she was 33 weeks and 3 days old, when she was delivered. The result was a live male newborn weighing 2,255 g (AGA, 64th percentile), height 41 cm, Apgar 8 1min to 9 5min (Figure 3). He was hospitalized in the neonatology department where he remained for 15 days, being discharged in perfect condition and, at the date of this manuscript, he has completed 3 months without alterations in his psychomotor development (Figure 4).
Discussion
The TRAP sequence is an alteration of the fetal circulation in monochorionic twin gestations where the presence of arterio-arterial (A-A) and veno-venous (V-V) anastomoses give rise to a retrograde perfusion phenomenon with delayed cardiac function of one of the twins during embryogenesis3. The so-called 'pump' twin as-sumes its hemodynamic load and that of its 'acardiac' sibling, which can lead to complications such as congestive heart failure, fetal hydrops, premature delivery and even intrauterine death2,3.
Prenatal diagnosis in the TRAP sequence is performed by two-dimensional ultrasound and con firmed by color Doppler. However, the presence of fetal heartbeats in the acardiac fetus does not rule out the diagnosis4.
Among the therapeutic options, the use of intrafetal ablation techniques is currently preferred, among which radiofrequency ablation (RFA) - a procedure not yet available in Peru - and intrafetal laser ablation stand out. The latter is a simple, safe, effective and more accessible technique compared to other techniques and can be performed on an outpatient basis6,8.
This is the first application of intrafetal laser therapy in Peru in a pregnant woman with a biamniotic monochorionic twin pregnancy with a diagnosis of TRAP sequence with a reserved prognosis, due to the 'acardiac' twin/'pump' twin (GA/GB) weight ratio of 64%. Therefore, the intervention was scheduled 2 weeks later when the GA/GB weight ratio progressed to 92%9, considering that an increase of more than 70% requires an intervention due to the poor prognosis4. The patient presented premature rupture of membranes, one of the most frequent complications of this type of procedure. However, the absence of procedure-related complications during or within 48 hours after the intervention has been reported in pregnancies with an average gestational age of 13 weeks and 5 days, as well as a fetal survival rate of 92%, suggesting that early intrafetal laser therapy (12-14 weeks) does not increase the rate of fetal loss, but may even be advantageous with respect to initiating a late intervention (16-19 weeks)10,11. And, although its neonatal survival rate is comparable with RFA applied before 16 weeks, the incidence of PROM before 32 weeks of gestation for this technique is significantly higher12.
The patient remained hospitalized until 33 weeks 3 days and had a preterm delivery by elective cesarean section, a complication found by other authors in previous studies7,8. The newborn did not present neurological alterations up to the time of hospital discharge on the 15th day. However, neurodevelopmental alterations may occur in surviving twins in up to 6.8%, so it is suggested to perform pre- and postnatal brain imaging studies in these newborns to rule out severe brain injury, together with a standardized follow-up ideally at 2, 5 and 8 years, to have a reliable view of long-term infant development13.
In summary, we report the first case of TRAP sequence treated prenatally using the intrafetal laser technique in a private center in Lima, Peru, with a successful outcome, highlighting its efficacy, simplicity, low cost, and outpatient approach. Furthermore, we believe it is necessary to implement this technique as a treatment that in the long term will reduce the economic and social costs for the health system and will improve the survival prognosis of the pump twin.
REFERENCES
1. van Gemert MJC, van den Wijngaard JPHM, Vandenbussche FPHA. Twin reversed arterial perfusion sequence is more common than generally accepted. Birth Defects Res A Clin Mol Teratol. 2015;103(7):641-3. https://doi.org/10.1002/bdra.23405 [ Links ]
2. Herrera TT, Rueda K, Espinosa H, Britton GB. Intestinal volvulus in the pump twin of a twin reversed arterial perfusion (TRAP) sequence after laser therapy at 18 weeks: a case report. J Med Case Reports. 2020;14(1):123. https://doi.org/10.1186/s13256-020-02444-3 [ Links ]
3. Shettikeri A, Acharya V, V S, Sahana R, Radhakrishnan P. Outcome of Pregnancies Diagnosed with TRAP Sequence Prenatally: A Single-Centre Experience. Fetal Diagn Ther. 2020;47(4):301-6. https://doi.org/10.1159/000503389 [ Links ]
4. Vitucci A, Fichera A, Fratelli N, Sartori E, Prefumo F. Twin Reversed Arterial Perfusion Sequence: Current Treatment Options. Int J Womens Health. 2020;12:435-43. https://doi: 10.2147/IJWH.S214254 [ Links ]
5. Emery SP, Bahtiyar MO, Moise KJ. The North American Fetal Therapy Network Consensus Statement: Management of Complicated Monochorionic Gestations. Obstetrics & Gynecology. 2015;126(3):575-84. https://doi: 10.1097/AOG.0000000000000994 [ Links ]
6. Tan TYT, Sepulveda W. Acardiac twin: a systematic review of minimally invasive treatment modalities. Ultrasound Obstet Gynecol. 2003;22(4):409-19. https://doi.org/10.1002/uog.224 [ Links ]
7. Shaw CJ, Paramasivam G, Vacca C, Lees CC. Expectant management versus multifetal pregnancy reduction in dichorionic triamniotic (DCTA) triplets: Single centre experience. Eur J Obstet Gynecol Reprod Biol. 2021;264:200-5. https:// doi.org/10.1016/j.ejogrb.2021.07.021 [ Links ]
8. Seshadri S, Shinde RR, Ram U. Intrafetal laser for midtrimester TRAP sequence-experience from a single center. Prenat Diagn. 2020;40(7):885-91. https://doi.org/10.1002/pd.5707 [ Links ]
9. Wong AE, Sepulveda W. Acardiac anomaly: current issues in prenatal assessment and treatment. Prenat Diagn. 2005;25(9):796-806. https://doi.org/10.1002/pd.1269 [ Links ]
10. Tavares de Sousa M, Glosemeyer P, Diemert A, Bamberg C, Hecher K. First-trimester intervention in twin reversed arterial perfusion sequence. Ultrasound Obstet Gynecol. 2020;55(1):47-9. https://doi.org/10.1002/uog.20860 [ Links ]
11. Chaveeva P, Poon LC, Sotiriadis A, Kosinski P, Nicolaides KH. Optimal method and timing of intrauterine intervention in twin reversed arterial perfusion sequence: case study and meta-analysis. Fetal Diagn Ther. 2014;35(4):267-79. https:// doi.org/10.1159/000358593 [ Links ]
12. Pagani G, D'Antonio F, Khalil A, Papageorghiou A, Bhide A, Thilaganathan B. Intrafetal laser treatment for twin reversed arterial perfusion sequence: cohort study and meta-analysis. Ultrasound Obstet Gynecol. 2013;42(1):6-14. https://doi.org/10.1002/uog.12495 [ Links ]
13. van Klink J, Koopman H, Middeldorp J, Klumper F, Rijken M, Oepkes D, et al. Long-term neurodevelopmental outcome after selective feticide in monochorionic pregnancies. BJOG: Int J Obstet Gy. 2015;122(11):1517-24. https://doi.org/10.1111/1471-0528.13490 [ Links ]
Received: March 23, 2022; Accepted: September 03, 2022











 text in
text in 





